Abstract
People who suffer from asthma can have difficulty breathing after they are exposed to normally harmless substances in the air, such as pollen, dust, smoke, and pet dander. Some people experience a worsening of their asthma symptoms after a thunderstorm, and data tell us that climate change is making asthma more of a problem. But how do weather and climate events make it hard for some people to breathe? Asthma happens when the body’s immune system mistakes airborne particles for dangerous invaders and tries to fight them. It seems that climate change is increasing the amounts of air pollution, pollen, and mold in the air. The more of these triggers people breathe in, the greater the risk of asthma. In this article, we will explain how asthma happens, how climate change is making it worse, and what we can all do to help.
Imagine lying in bed on a sweltering summer night. You suddenly feel a cool, refreshing breeze blowing in through the open window—aaahh! A few minutes later, a driving rain begins to fall, and the wind gusts grow stronger. As you get up to close the window, you are startled by a sudden bright flash, followed closely by the crash of thunder—a summer storm! How does this make you feel? Do you enjoy these dramatic displays of nature’s power, or do you find them to be an unpredictable, scary part of summer? Reactions to thunderstorms can go beyond “love them” vs. “hate them”. Did you know that under certain circumstances, thunderstorms can make some people physically sick? Although it is rare, individuals with a troublesome breathing condition called asthma sometimes find that their symptoms begin or get worse after thunderstorms. This is called thunderstorm asthma, and we think that climate change might make this rare condition happen more often!
In this article, we will explain what asthma is, how climate change might be making it worse, and what can be done—in both the short and long term—to help protect human health in the face of Earth’s changing climate.
What is Asthma?
Think of your lungs as two big balloons inside your chest. When you breathe, air goes in and out of these balloons through tiny tubes called airways. In people with asthma, the airways can become swollen, narrow, and filled with mucous. This makes it hard to breathe—like trying to drink a thick milkshake through a skinny straw. Asthma symptoms include breathlessness, coughing, wheezing, and tightness in the chest, and these symptoms can be triggered by things in the environment, such as dust, pollen, smoke, and animal dander.
But why does exposure to these common particles trigger asthma…and why does it happen in some people but not others? Our bodies have a special system called the immune system, which helps protect us from germs and other harmful things. Sometimes the immune system can get a little mixed up. The immune system of a person with asthma mistakenly treats things like dust, pollen, or pet hair as dangerous invaders, and tries to fight them (Figure 1). Specifically, certain immune system cells release a substance called IgE, which sticks to other important immune cells called mast cells. Mast cells are found in many places in the body, including the lungs. When a person with asthma breathes a trigger like pollen or dust into their lungs, the IgE stuck to the mast cells recognizes the trigger and sends a danger signal into the mast cells, telling them to release a chemical called histamine. You may be familiar with the word histamine from “antihistamines”. These are medicines commonly used to stop annoying allergy symptoms like sneezing, itchy eyes, and runny nose—which are caused by histamine. In people with asthma, histamine causes the airways to become swollen, narrow, and clogged with mucous, making it hard for air to pass through them. If you think of the airways like a garden hose, when everything is normal, water flows easily through the hose. But if someone were to step on the hose, the water would not flow well. In asthma, histamine is like that foot stepping on the hose, making it hard for air to flow into the lungs and causing the symptoms described above.
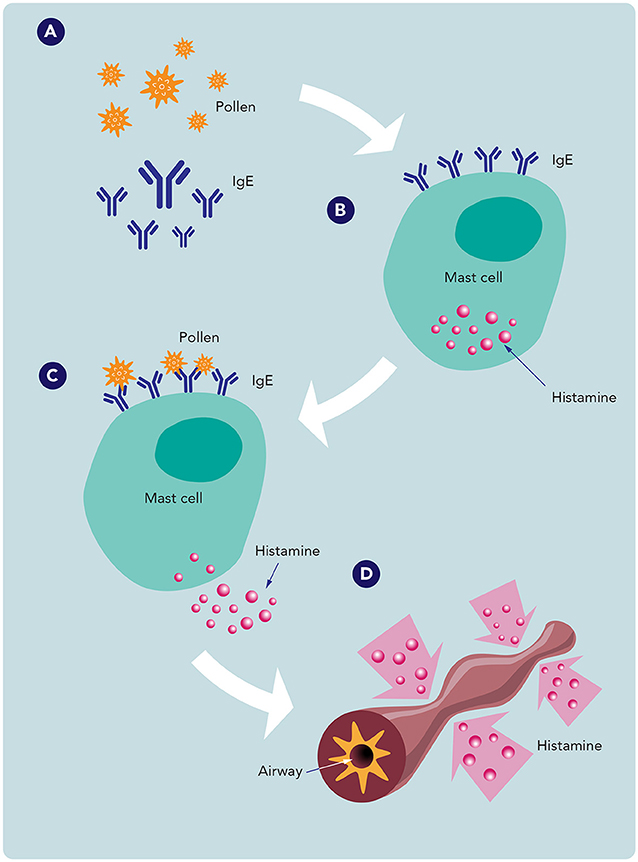
- Figure 1 - In people with asthma, the immune system treats things like pollen and other generally harmless substances like dangerous invaders.
- (A) In the presence of these substances, certain cells of the immune system produce a substance called IgE. (B) IgE can stick to other immune cells, called mast cells, found in many parts of the body including the lungs. (C) Then the pollen binds to the IgE on mast cells and triggers them to release histamine. (D) Among other effects, histamine causes the airways to become swollen, narrow, and clogged with mucus, making it difficult to breathe.
Climate Change and Human Health
These days, pretty much everyone understands that climate change is causing serious problems for our planet. As global temperatures rise, weather patterns are changing all over the world. Some places are getting hotter while other places are experiencing colder winters. Glaciers and ice sheets are melting, raising sea levels. Severe weather events including heatwaves, droughts, wildfires, and floods are happening more often and getting more intense.
These climate changes are clearly harmful for many of Earth’s species, including humans. Some plant and animal species are struggling to survive as their ecosystems change and, if you watch the news, you know that severe weather events can injure and even kill many people. But in addition to these direct effects on human health, scientists are also starting to see increases in asthma and other disorders of the immune system that appear to be linked to the changing climate [1, 2]. But how? The connection is still under intense investigation, but evidence suggests that climate change is increasing the amounts of substances in the environment that trigger asthma in sensitive individuals—especially pollen, air pollution, and mold.
Climate Change is Increasing Pollen
Pollen, the powdery substance made by some plants to help them reproduce, is a common trigger for asthma and allergies. Not surprisingly, more pollen in the environment often means more (or worse) asthma [3]. Climate change increases pollen in several ways. The first mechanism involves carbon dioxide (CO2). Human activities, like burning fossil fuels, pump large amounts of CO2 into the atmosphere. You have probably heard that CO2 contributes to global warming by trapping the sun’s heat near the Earth, but that is not all—higher levels of CO2 seem to increase the amount of pollen in the air, too. For example, one study showed that ragweed plants produced 61% more pollen when CO2 concentrations were doubled [4]. Warmer temperatures are also associated with higher pollen concentrations. Some scientists think that warming temperatures may increase pollen concentrations by as much as 200% by the end of this century [5].
Thunderstorm asthma may also be explained by pollen. During a storm, the winds sweep pollen up into the clouds, where high humidity and the energy of lightning break up the pollen particles, making them more likely to enter deep into the airways and start the dangerous chain of immune events leading to asthma symptoms [6]. If climate change results in more pollen and more thunderstorms, it seems likely that we will see an increase in thunderstorm asthma if climate change worsens (Figure 2).
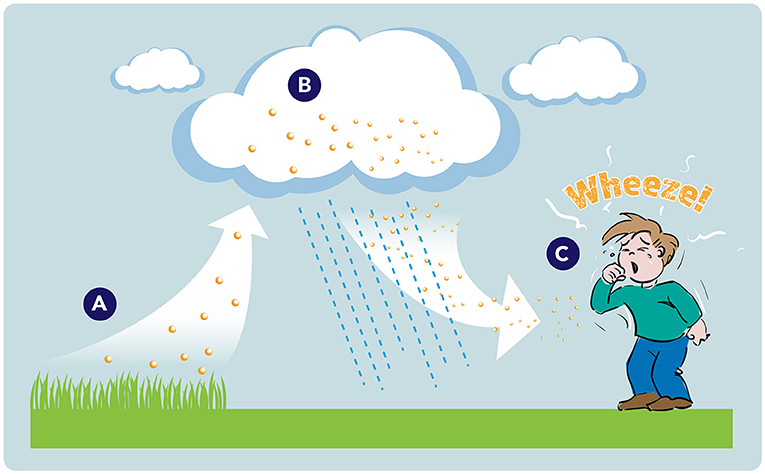
- Figure 2 - People who suffer from thunderstorm asthma find that their symptoms start or get worse after a thunderstorm.
- (A) During a storm, pollen is carried up into the clouds by the wind. (B) In the clouds, the moisture and energy of lightning break up the pollen particles into a form that can easily enter deep into a person’s airways. (C) When winds carry the broken-up pollen particles back to ground level, people can breathe them in, triggering asthma.
“Dirty” Air Makes Asthma Worse
While you probably know that air pollution can contribute to climate change, did you know that climate change can make air pollution worse, too? Air pollution happens when certain dangerous gases and tiny particles, called particulate matter (PM), get into the air. Particulate matter is made up of many things—for example dust, dirt, soot, and smoke. Hot weather can trap bad stuff like car exhaust and factory smoke close to the ground, increasing the amount of PM that people breathe in—especially in big cities. Warmer temperatures and droughts also dry out forests and grasslands, leading to more frequent wildfires that fill the air with dust and thick smoke, which contain lots of PM and can travel long distances. Wildfires are currently believed to produce at least 25% of the PM found in Earth’s atmosphere [7]. PM can make asthma worse, so people with asthma may notice that it is harder to breathe when it is hot outside or when there are big wildfires burning, even if they are relatively far away.
More Wet Weather Means More Mold
Have you ever seen green or black fuzzy stuff growing on old bread or damp walls? That is mold! Mold loves warm, wet places. Climate change is making some parts of the world warmer and rainier, creating perfect conditions for mold growth. As mold grows, it releases tiny particles, called spores, into the air. Warmer temperatures can increase spore production. Airborne mold spores can be easily inhaled, triggering asthma in some people. While mold growing in the outdoor environment can cause asthma, indoor mold is a big problem, too. If buildings are not properly protected from wet weather, mold can grow in any areas that stay damp. Since climate change is leading to increased flooding and extreme rainfall, mold growth may increase in homes that are not well protected against the weather. It is estimated that 21% of asthma cases are due to indoor dampness and mold [8]. Floods and storms can increase fungal spores, which are associated with thunderstorm asthma.
Everything is Connected… and Everyone Can Help
Unfortunately, asthma is only one example of how climate change might act on the immune system to cause health problems. Allergies, autoimmune disorders (e.g., rheumatoid arthritis, multiple sclerosis, and Crohn’s disease), and even some cancers might be increasing in response to Earth’s changing climate [9, 10]. To keep people healthy and to protect the planet for future generations, the entire world must take action now.
Humans generally do not harm the Earth on purpose. Most of the damage that we cause happens as we try to meet our growing needs for space, food, and natural resources. The problem is that we humans are so focused on meeting our own needs that we often do not pay attention to the negative impact our actions have on the Earth—until it is too late. If we want to heal the planet, we must remember that the health of humans, animals, and the environment are all connected. We must figure out how to balance our own needs with those of other animals and the environment (plants, water, and air) (Figure 3).
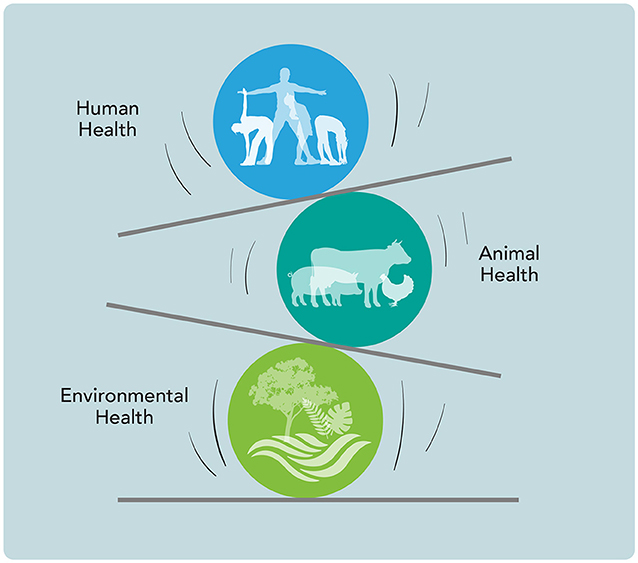
- Figure 3 - The health of humans, animals, and the environment are all connected.
- To heal the damage humans have done to the planet and protect future generations from diseases caused by climate change, we must figure out how to balance our own needs with the needs of all other species and the health of Earth’s ecosystems.
To reduce the impact of climate change on human health, both short- and long-term solutions are needed. First, climate change is already affecting human health, so we must take steps to protect people. This short-term approach is called adaptation. In terms of helping people with asthma, adaptation can involve things like using air filters in our homes to decrease pollen and other PM, and protecting buildings against dampness and mold. In the longer term, we must also consider mitigation—battling climate change directly, by cutting or preventing greenhouse gas emissions to limit global warming.
Neither adaptation nor mitigation are easy—especially if we want to protect all people regardless of where they live, their economic status, or their race. We will need the cooperation of all countries and collaboration between many kinds of scientists and other experts. But the difficulty of this challenge should not prevent each of us from doing our part—we can all do something, and small actions can add up to big results. So, remember to recycle, use public transportation if possible, conserve energy, and most importantly, do not lose hope. Tell your friends and family what you have learned about how climate change is damaging human health, and join them in supporting organizations and government officials who respect the planet. (For more info, see this site.) Any steps we take to keep the Earth healthy will ultimately result in healthier, happier living things, including humans!
Glossary
Asthma: ↑ A lung condition in which the airways swell up, narrow, and fill with mucus, making it hard to breathe. Symptoms include coughing, wheezing, and feeling out of breath. See here.
Immune System: ↑ The body’s defense against germs and other harmful substances. It is made up of special cells, tissues, and organs that work together to protect us from illness and infection.
Mast Cells: ↑ Special immune cells found in many parts of the body that help the body fight diseases. When activated, mast cells release a chemical called histamine that causes allergy and asthma symptoms.
Histamine: ↑ A chemical released by mast cells that causes allergy symptoms like sneezing, runny nose, and itchy eyes. In asthma, histamine makes the airways swollen and narrow, making it hard to breathe.
Particulate Matter: ↑ Tiny particles of dust, dirt, smoke, and soot in the air, which can get into the lungs and cause breathing problems. Climate change increases particulate matter from car exhaust, factories, and wildfire smoke.
Spores: ↑ Tiny cells produced by some plants, fungi, and microorganisms that can survive under very tough conditions and then grow into a new organism when conditions are favorable.
Adaptation: ↑ Taking action to protect people from the health effects of climate change that are happening now. Actions include using air filters, weatherizing buildings, and preparing for severe weather events.
Mitigation: ↑ Reducing climate change by limiting greenhouse gases, including by cutting emissions from cars and power plants. Mitigation tackles the root cause of climate change to prevent future harm.
Acknowledgments
Co-written by Susan Debad Ph.D., graduate of the University of Massachusetts Graduate School of Biomedical Sciences (USA) and scientific writer/editor at SJD Consulting, LLC. Ioana Agache, Cezmi Akdis, Mubeccel Akdis, Ali Al-Hemoud, Isabella Annesi-Maesano, John Balmes, Lorenzo Cecchi, Athanasios Damialis, Tari Haahtela, Adam L. Haber, Jaime E. Hart, Marek Jutel, Yasutaka Mitamura, Blandina T. Mmbag, Jae-Won Oh, Abbas Ostadtaghizadeh, Ruby Pawankar, Mary Prunicki, Harald Renz, Mary Rice, Nelson Augusto, Rosario Filho, Chrysanthi Skevaki, Francis Thien, Claudia Traidl-Hoffmann, and Gary W.K. Wong were co-authors on the original manuscript. Funding was provided by the John Rock Professorship, and NIH grants P01 HL152953, R01 ES032253, U01 AI147462, and U01AI140498.
Conflict of Interest
KN currently reports grants from National Institute of Allergy and Infectious Diseases (NIAID), National Heart, Lung, and Blood Institute (NHLBI), National Institute of Environmental Health Sciences (NIEHS); Stock options from IgGenix, Seed Health, ClostraBio, Cour, Alladapt; Consultant for Excellergy, Red tree ventures, Regeneron, and IgGenix; Co-founder of Alladapt, Latitude, and IgGenix; National Scientific Committee member at Immune Tolerance Network (ITN), and National Institutes of Health (NIH) clinical research centers; patents include, “Mixed allergen com-position and methods for using the same,” “Granulocyte-based methods for detecting and monitoring immune system disorders,” and “Methods and Assays for Detecting and Quantifying Pure Subpopulations of White Blood Cells in Immune System Disorders.” VS reports no COI.
Original Source Article
↑Agache, I., Akdis, C., Akdis, M., Al-Hemoud, A., Annesi-Maesano, I., Balmes, J., et al. 2024. Immune-mediated disease caused by climate change-associated environmental hazards: mitigation and adaptation. Front. Sci. 2:1279192. doi: 10.3389/fsci.2024.1279192
References
[1] ↑ Asher, M. I., Rutter, C. E., Bissell, K., Chiang, C. Y., El Sony, A., Ellwood, E., et al. 2021. Worldwide trends in the burden of asthma symptoms in school-aged children: global Asthma Network Phase I cross-sectional study. Lancet 398:1569–1580. doi: 10.1016/S0140-6736(21)01450-1
[2] ↑ Gutowska-Slesik, J., Samoliński, B., and Krzych-Fałta, E. 2023. The increase in allergic conditions based on a review of literature. Postepy Dermatol. Alergol. 40:1–7. doi: 10.5114/ada.2022.119009
[3] ↑ Annesi-Maesano, I., Cecchi, L., Biagioni, B., Chung, K. F., Clot, B., Collaud Coen, M., et al. 2023. Is exposure to pollen a risk factor for moderate and severe asthma exacerbations? Allergy 78:2121–2147. doi: 10.1111/all.15724
[4] ↑ Wayne, P., Foster, S., Connolly, J., Bazzaz, F., and Epstein, P. 2002. Production of allergenic pollen by ragweed (Ambrosia artemisiifolia L.) is increased in CO2-enriched atmospheres. Ann. Aller. Asthma Immunol. 88:279–282. doi: 10.1016/S1081-1206(10)62009-1
[5] ↑ Zhang, Y., and Steiner, A. L. 2022. Projected climate-driven changes in pollen emission season length and magnitude over the continental United States. Nat. Commun. 13:1–10. doi: 10.1038/s41467-022-28764-0
[6] ↑ Sampath, V., Aguilera, J., Prunicki, M., and Nadeau, K. C. 2023. Mechanisms of climate change and related air pollution on the immune system leading to allergic disease and asthma. Semin. Immunol. 67:101765. doi: 10.1016/j.smim.2023.101765
[7] ↑ Burke, M., Driscoll, A., Heft-Neal, S., Xue, J., Burney, J., Wara, M., et al. 2021. The changing risk and burden of wildfire in the United States. Proc. Natl. Acad. Sci. 118:e2011048118. doi: 10.1073/pnas.2011048118
[8] ↑ Mudarri, D., and Fisk, W. J. 2007. Public health and economic impact of dampness and mold. Indoor Air 17:226–235. doi: 10.1111/j.1600-0668.2007.00474.x
[9] ↑ The Lancet Oncology 2023. Climate change and skin cancer: urgent call for action. Lancet Oncol. 24:823. doi: 10.1016/S1470-2045(23)00348-0
[10] ↑ Miller, F. W. 2023. The increasing prevalence of autoimmunity and autoimmune diseases: an urgent call to action for improved understanding, diagnosis, treatment, and prevention. Curr. Opin. Immunol. 80:102266. doi: 10.1016/j.coi.2022.102266
