Abstract
I am a medical doctor who treats women during pregnancy and childbirth. I aspire to give them the best possible care, based on scientific evidence. In this article, I will explain how we do scientific experiments in medicine and how we use the results to improve healthcare. I will then tell you about an important relationship I found between calcium intake and high blood pressure in pregnant women, and how this discovery is being used to improve pregnant women’s health and even save their lives. Finally, I will share with you some of my hopes for a future of healthcare that is supported by science and benefits everyone.
Dr. José Belizán is the winner of the 2023 John Dirks Canada Gairdner Global Health Award, for his work developing cutting-edge and low-cost treatments for mother and baby health during pregnancy and the first 12 months after childbirth (the “perinatal period”). His work improved wellbeing and care, reduced diseases and deaths, and ensured everyone could benefit equally, including those without healthcare insurance or with low incomes.
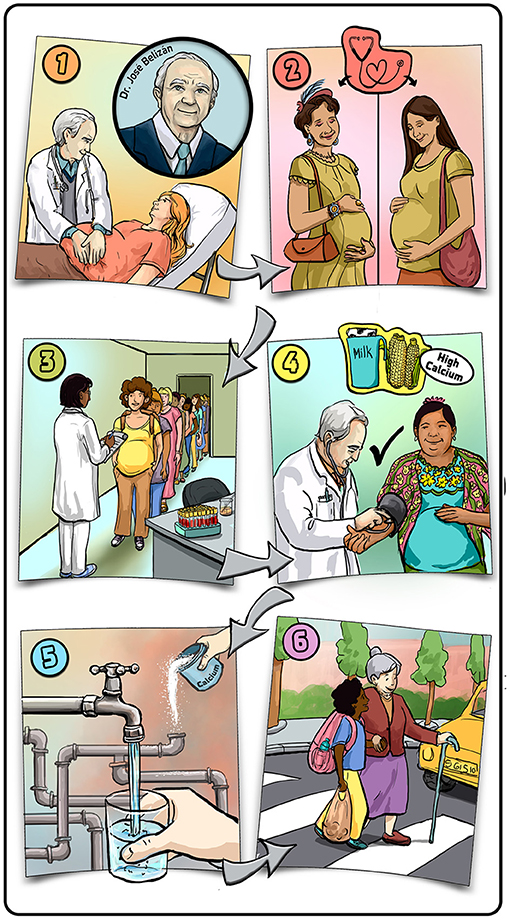
- Graphical Abstract - (1) I am a doctor taking care of pregnant women.
- (2) I try to provide the best medical care to all pregnant women from all backgrounds. (3) I use a scientific process called randomized controlled trials to check whether new treatments can improve upon existing treatments. (4) In studies I did in Guatemala, I found a relationship between calcium intake and a dangerous condition that can occur during pregnancy called preeclampsia. Based on my research, experts instructed that most people, and especially pregnant women, should increase their calcium intake. (5) One way to increase a population’s calcium intake is to add calcium to drinking water. (6) For me, helping others is the most gratifying thing I can do. Illustration by: Iris Gat.
The Role of Doctors
I am a medical doctor. My specialty is obstetrics—throughout my career, I have been trying to provide pregnant women with the best possible healthcare during pregnancy and birth (note: in this article, we use the term “pregnant women” to refer to any person who is carrying a female reproductive system). My role as a doctor is to improve the lives of the people around me and, in some cases, even to save lives. I do that by providing care for patients, easing their pain, and trying to improve the quality of patient care. You might be aware that the socio-economic status of people—meaning the life conditions that they have—greatly affects the quality of medical treatment that they normally get. People with high socio-economic status (for example, many people in Canada, the United States, and Europe) usually receive good health care. Unfortunately, people with low socio-economic status (for example, many people in Africa and in Latin America) often do not have access to proper health care. As a doctor treating women in South America, one of my personal missions is to promote equity in healthcare and make sure that everyone gets the best possible treatment, irrespective of their socio-economic status.
To provide the best possible treatments to my community, I need to know the needs, wants, and concerns of the population regarding their health and the healthcare they receive. To improve the healthcare that I provide to the women in my population, I first try to find out what bothers them about current healthcare practices. Then I come up with possible changes that could be made to improve existing practices, and I ask the women which of these potential new treatments they might be willing to receive. Finally, before changing the current healthcare practices, I conduct scientific research to check whether the new practice is indeed better than the old one. Importantly, I try to develop procedures that will be inexpensive, so that no woman will be unable to afford proper care.
Improving Medical Care With Science
When I was a medical student a few decades ago, I was concerned about the quality of medical care provided to women in my community. I noticed that some medical practices and procedures that obstetricians did were uncomfortable or painful for women and were not backed up by science (for example, cesarean section as you will see later on). In other words, there was no scientific evidence proving that these practices cause more benefit than harm or that they were better than other practices that might not bother the women as much. In many cases, these procedures became routine just because a well-respected doctor said the procedures work. But one doctor’s opinion—no matter how respected that doctor is—is not enough to prove that a certain procedure is better than all other possibilities. Various doctors, myself included, realized that a better, more scientific method should be developed to measure how well medical procedures work. We wanted to provide medical care based on evidence, not opinions.
Some of us started doing what are called randomized controlled trials (Figure 1), which are experiments used to determine scientifically whether a medical practice works [1]. Let us say there is a new drug (or any kind of treatment) that we want to test to see if it should become the common practice for preventing or treating a medical condition. We take a group of people with the medical condition we are studying and assign half of them to receive the new treatment. The other half does not receive the treatment. Importantly, the choice of who receives the treatment and who does not is random. In the case of a drug, there is usually one pill that contains the active medicine that we want to test and another pill that looks exactly the same but does not contain the active medicine. The second pill is what we call a placebo. None of the people know which pill they are getting, and even the doctor that gives the participants the pills does not know which pills were assigned to which person. After everyone takes the pills for the prescribed time, medical tests are done (for example, measuring blood pressure) and statisticians analyze the data to see if improvements resulted from taking either pill. If statistics show that there were significant improvements among people who took the active pill compared to people who took the placebo, then the new drug is determined to be effective for the disease being studied.
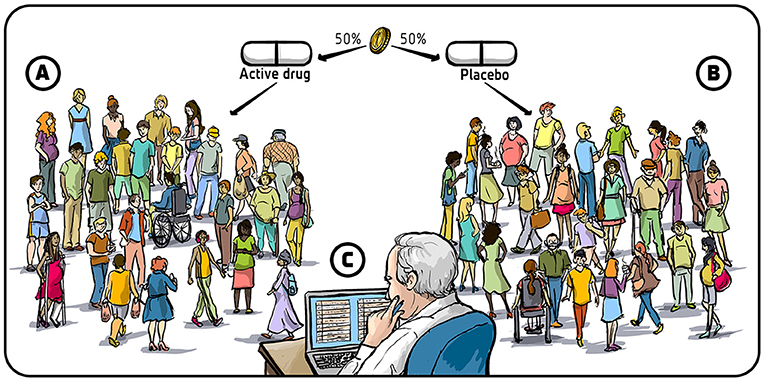
- Figure 1 - Randomized controlled trials.
- In randomized controlled trials, (A) a randomly selected half of the tested population is treated with an active drug, and (B) the other half is treated with a placebo. (C) After the treatment, the data are studied using a type of math called statistics, to see if taking the active drug significantly improved the condition of the patients compared to the group that took the placebo. The drug is only considered a potential new treatment for the condition if its use led to significant improvement. Illustration by: Iris Gat.
Discovery About Calcium in Pregnancy
During pregnancy, some women have a complication called preeclampsia [2]. In this condition, the pregnant woman’s blood pressure rises during the second half of the pregnancy (Figure 2A). Preeclampsia is a dangerous condition, as it can lead to damage of internal organs of the mother, including the kidneys, liver, lungs, heart, and even the brain. If preeclampsia develops further, it can become an even more dangerous condition called eclampsia, in which pregnant women experience seizures and can die. Until recently, there was no preventive treatment for preeclampsia, and tens of thousands of women around the world died from the condition each year. Doctors knew that giving birth to the child could cure preeclampsia, but in many cases the preeclampsia happened too early in the pregnancy, when the baby was too premature to be born safely.
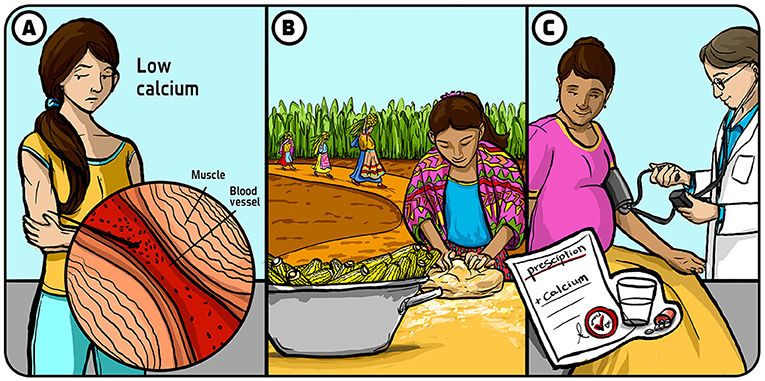
- Figure 2 - Calcium intake and health.
- (A) When calcium intake is low, the body sends a message to the cells to store what little calcium is taken in with food. When muscles store calcium, they contract and squeeze the blood vessels they surround, increasing blood pressure. (B) When I worked in Guatemala, I noticed that pregnant women there rarely experienced preeclampsia during pregnancy. After some studies, I found that these women had high calcium intake because their diets were based on lime treated corn. (C) As a result of my studies, it has now become standard for pregnant women to be supplemented with calcium during pregnancy. Illustration by: Iris Gat.
In the 1970s, I was working in Guatemala in Central America. I noticed preeclampsia occurred only rarely among Guatemalan women, much less often than among women with the same socio-economic status from other countries. That surprised me because many of these women were poor and did not have access to good medical care. As I started to study this interesting observation, I realized that the Guatemalan women were eating a Mayan diet that was heavily based on corn (Figure 2B) [3]. Treatment of corn before milling implied soaking corn in lime water resulting in a high concentration of calcium, so I wondered if there could be a relationship between calcium intake and preeclampsia. To test this, my colleagues and I conducted randomized controlled trials where we measured women’s calcium intake and eventually proved that women who took extra calcium during pregnancy had a significantly lower risk of suffering from preeclampsia (Figure 2C) [4]. Over time, many other researchers replicated our results and eventually—after professional discussions by a group of experts—the World Health Organization made a strong recommendation that pregnant women should be supplemented with calcium to prevent preeclampsia.
We now know that when there is not enough calcium in the body, a message is sent to the cells to store up the calcium they do have. This means that the muscles, including those surrounding blood vessels, take in the calcium that is eaten in food. When muscles take in calcium they contract more, and these contractions squeeze the blood vessels, leading to an increase in blood pressure. On the contrary, if there is too much calcium in the blood it is removed from the body through urine and does not cause any problems.
There are several reasons why people, specifically pregnant women, might not get enough calcium. One reason is that, for many people, calcium is not available in their diets. About three billion people around the world do not have access to foods containing sufficient amounts of calcium. Even in places where calcium-containing foods are available, it can be very difficult to get people to eat enough of these calcium-rich foods, even if they are recommended by experts. Also, sometimes the media leads people to have a specific perception about certain foods. For example, in the US, there was a trend against consuming milk. The argument was that many people experience digestion issues from consuming lactose (the main sugar in milk). In fact, only few people have lactose intolerance, and many people could benefit from consuming milk because it has a high calcium content. This is an example of why it is important to question dietary recommendations that you see in the media. Instead, you should talk to experts who have the proper training based on scientific evidence, and can see the bigger picture.
To help increase calcium intake in populations where calcium is not readily available, calcium can be included in products such as wheat and water. This is called a population-level intervention—we try to raise the calcium intake of the whole population. Importantly, this intervention is not very expensive and could save many lives worldwide. To develop this intervention, we first work in the laboratory to find the best ways to enrich water with calcium. Then, we do tests to see how much calcium we can add to the water without it making it taste bad. Finally, we add calcium to the water and see how much it improves the calcium intake of a tested population. In populations that normally have a low calcium intake, we know that raising the calcium intake for pregnant women can reduce the occurrence of preeclampsia by half or more. This can significantly reduce deaths of pregnant women around the world.
The Future of Maternal Healthcare
My hope is that, in the future, more of the medical procedures that are used will be based on evidence. Some procedures that are currently still used have been scientifically proven to be more harmful than beneficial. Cesarean sections are an important example. A cesarean section is a surgery that is done to deliver a baby. In principle, cesarean sections should only be done when natural delivery is not possible or puts the mother or the baby at risk. Unfortunately, cesarean sections are used far more than they should be—not because women prefer them over natural delivery, but because it is easier for the doctors. But performing cesarean sections can have various negative effects on women, both in their current pregnancy and in future pregnancies, as well as on the children that are delivered that way [5]. In addition, women can feel sad and stressed if they must undergo a procedure they do not want. This example tells us that it is very hard to change the behaviors and routines of medical doctors, even if those changes are supported by clear scientific evidence.
We still have not been as successful as we would like to be in terms of reducing the number of cesarean sections done around the world, but we keep working on it. In addition to talking with doctors, we also educate women to let them know that they have the right to choose a natural delivery despite what their doctors say. I hope that, with time, we can make both doctors and women aware of the scientific knowledge that can greatly improve the healthcare women receive during pregnancy and delivery. For me, the most gratifying thing in life is to know that I have done something for other people and for the community. We can help people in many ways. I chose to do so through medicine, which is a human-centered profession, but you might choose to do it in other ways. In the world of medicine, we definitely need more people who are searching for ways to improve medical care, particularly for populations that currently do not have the financial means to afford private health care.
Glossary
Obstetrics: ↑ A field of medicine that deals with pregnancy and childbirth.
Socio-economic Status: ↑ The life conditions that people experience in terms of their education, income, and quality of life.
Equity: ↑ The situation in which everyone is treated fairly according to their needs and no group of people is given special treatment.
Randomized Controlled Trials: ↑ Experiments in which scientists test new things, like medicines or treatments, by dividing people into two groups and comparing the results fairly to see what works best.
Placebo: ↑ A pill or treatment given to patients as part of a randomized controlled trial, that does not contain any active medicine.
Preeclampsia: ↑ A dangerous condition that some women experience during pregnancy where they blood pressure rises and could lead to damage of internal organs.
Population-level Intervention: ↑ A population-based approach considers intervening at all possible levels of practice. Interventions may be directed at the entire population within a community.
Conflict of Interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
I wish to thank Noa Segev for conducting the interview which served as the basis for this paper and for co-authoring the paper, and Iris Gat for providing the figures.
Additional Materials
- Dr. Belizán Live Q&A - 2023 Canada Gairdner Awards Announcement (YouTube)
- Dr. Belizán’s Advice for Young Scientists - 2023 Canada Gairdner Awards Announcement (YouTube)
References
[1] ↑ Bhide, A., Shah, P. S., and Acharya, G. 2018. A simplified guide to randomized controlled trials. Acta Obstetr. Gynecol. Scand. 97:380–7. doi: 10.1111/aogs.13309
[2] ↑ Davey, D. A., and MacGillivray, I. 1988. The classification and definition of the hypertensive disorders of pregnancy. Am. J. Obstetr. Gynecol. 158:892–8. doi: 10.1016/0002-9378(88)90090-7
[3] ↑ Cormick, G., and Belizán, J. M. 2019. Calcium intake and health. Nutrients 11:1606. doi: 10.3390/nu11071606
[4] ↑ Belizán, J. M., Villar, J., Gonzalez, L., Campodonico, L., and Bergel, E. 1991. Calcium supplementation to prevent hypertensive disorders of pregnancy. N. Engl. J. Med. 325:1399–405. doi: 10.1056/NEJM199111143252002
[5] ↑ Belizán, J. M., Althabe, F., and Cafferata, M. L. 2007. Health consequences of the increasing caesarean section rates. Epidemiology 18:485–6. doi: 10.1097/EDE.0b013e318068646a
