Abstract
Systemic lupus erythematosus (SLE) is an autoimmune disease that affects multiple organ systems. Autoimmune diseases happen when the immune system attacks the body’s own cells instead of things like infections or cancers. Lupus is not a preventable disease and it can leave people with devastating symptoms that range from joint pain to kidney failure. It is important for patients to get an accurate diagnosis so that they can be treated as quickly as possible, to prevent further damage to the body’s tissues. In this article, we detail the four types of lupus: SLE, drug-induced, cutaneous, and neonatal lupus. We will also detail how lupus affects different organ systems. The diagnosis and treatment methods, including medications and lifestyle adjustments, are also highlighted. Additionally, it features a conversation with a lupus patient Miah who shares her journey and challenges living with this chronic condition, along with advice for others dealing with lupus.
Lupus: An Autoimmune Disease
The human immune system is programmed to help us fight against things that make us sick, like bacteria, viruses, and cancers. However, sometimes the immune system can become overactive and begin attacking the body’s own healthy tissue. This is called autoimmune disease. Systemic lupus erythematosus (SLE) is one of many autoimmune diseases. Lupus affects nearly five million people around the world, with 15% of those cases being kids under 18 [1]. To understand autoimmune diseases in general, we must figure out why they occur. Certain people are more likely to develop autoimmune diseases due to a combination of their genes and factors in their environments, like certain viruses, sunlight, pollution, smoking, or certain medicines [2].
Essentially, SLE can be triggered by any damage to cells that leads to cell death. In healthy people, their immune system usually clean up dead cells. In SLE, the immune system cannot clear the debris from the damaged cells, which then build up in the bloodstream. In response to the buildup of cell debris, the body calls on the B cells, which are cells of the immune system that help protect the body from harmful germs. B cells create antibodies, which are like tiny soldiers that normally fight against the germs that can make us sick. Some of the antibodies produced by the B cells stick to the dead cell parts and form clumps that are called immune complexes (Figure 1). These immune complexes then get stuck in various tissues such as the skin, joints, heart, and kidneys. Once these complexes land in the tissues, they cause an inflammatory response, which leads to the symptoms we see in SLE patients.
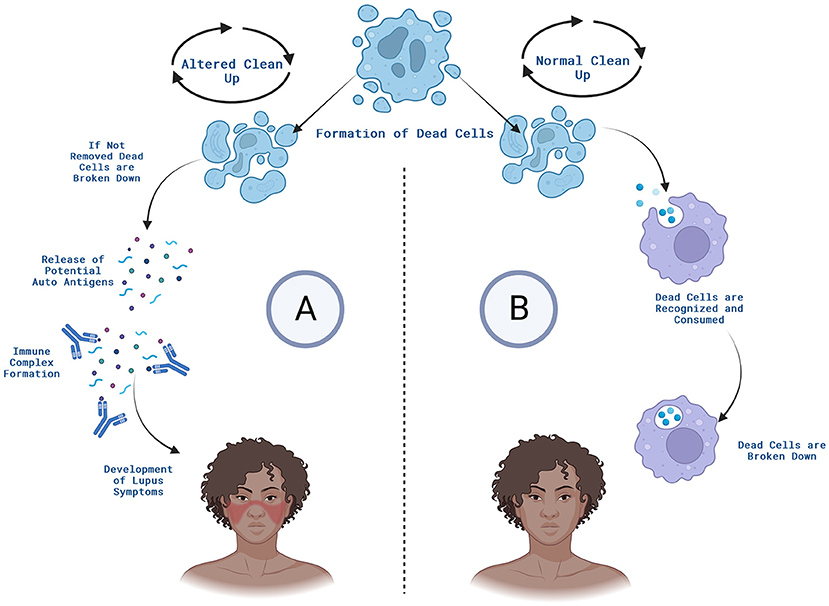
- Figure 1 - (A) In SLE, cells that are damaged by environmental factors like sunlight or heat can die, and the body’s immune system does not clean up the dead cell debris properly.
- B cells make antibodies that recognize this debris and stick it together into clumps called immune complexes. The immune complexes can end up in various organs, including the skin, contributing to the symptoms generally seen in SLE, like malar rash. (B) In the normal situation, when damaged cells die, certain cells of the body clean up the debris so no immune complexes are formed, and disease does not result. Created with BioRender.com.
Four Types of Lupus
There are four main types of lupus; SLE, drug-induced lupus, cutaneous lupus, and neonatal lupus. SLE is the most common type of lupus. It is a chronic condition, which means it will continue to worsen unless it is properly treated. Drug-induced lupus is caused by taking certain medications. It has similar symptoms to SLE, but the symptoms go away once the patient stops taking the medication. Cutaneous lupus happens when the immune system attacks the skin. Cutaneous lupus is often triggered by sun exposure that damages skin cells. Neonatal lupus occurs in babies born to a mother with an autoimmune disease such as lupus or Sjogren’s syndrome. The mothers’ autoantibodies cross the placenta and attack the developing baby [3]. Most cases of neonatal lupus go away within 6 months after the baby is born.
How Does Lupus Affect People?
SLE is a devastating disease that affects many of the body’s organ systems. People with SLE often experience symptoms that include fatigue, joint pain, and malar rash (Figure 2). Malar rash, also referred to as butterfly rash, is a red rash that goes across the bridge of the nose and the cheeks. In Latin, “lupus” means “wolf,” and it got its name from a 13th century doctor who thought the facial rash looked similar to a wolf’s bites. Patients can also have a discoid rash, which is a round, coin-shaped area that can lead to scarring. Discoid rash is more commonly seen in cutaneous lupus.
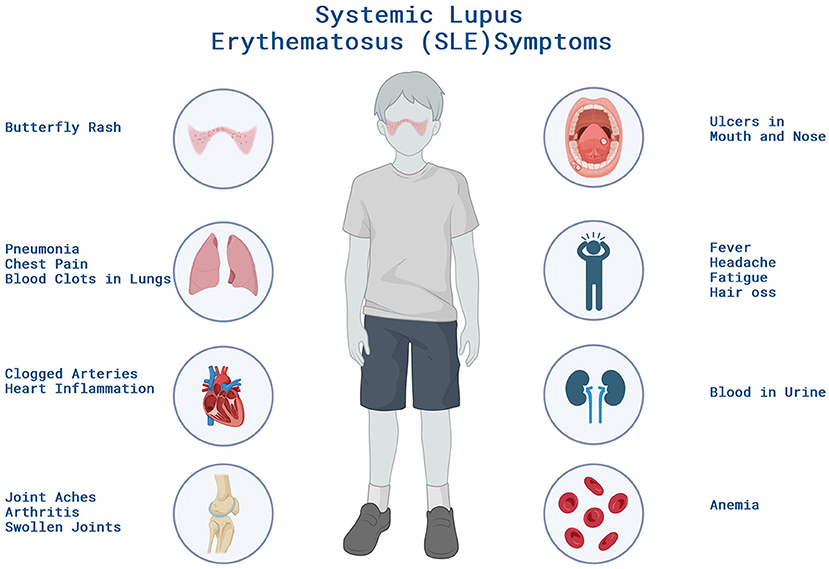
- Figure 2 - Patients with SLE can experience a variety of symptoms ranging from joint pain, rashes to organ inflammation impacting their health and daily life.
- These symptoms can increase in severity when the patient is experiencing a flare, which is a sudden worsening of symptoms. Created with BioRender.com.
The most common cause of death for SLE patients is lupus nephritis. Lupus nephritis happens when the immune complexes get stuck in the kidneys, which causes inflammation, scarring, and kidney damage. As a result, the kidneys can no longer filter the blood and transform the waste into urine. Decreased kidney function causes blood and protein in the urine as well as high blood pressure. Eventually, these patients require a procedure called dialysis, which does the kidneys’ job of removing toxins from the blood. In severe cases, patients need to get a kidney transplant.
How Is Lupus Diagnosed?
Doctors use a combination of blood and urine tests, signs and symptoms, and physical examination findings to confirm a lupus diagnosis. Testing for SLE-specific autoantibodies, including antibodies specific for human DNA is a reliable diagnostic tool. Regarding sign and symptoms a person is defined as having lupus if they meet four out of 11 common criteria: ulcers in the mouth, arthritis, sensitivity to light, blood disorders, kidney problems, DNA autoantibodies, immune system problems, brain disorders, and malar and discoid rashes [4].
How Is Lupus Treated?
The goal of SLE treatment is to suppress the overactive immune system. To manage the disease, physicians will often have the patient take a medicine called hydroxychloroquine, which was originally designed to fight some parasites but also weakens the body’s immune system, to protect healthy cells from being attacked [5]. Hydroxychloroquine blocks the production of autoantibodies, which reduces damage to healthy tissue.
SLE patients also experience flares of their symptoms, which means they have occasional spells of fatigue, joint pain, and dizziness. Physicians recommend anti-inflammatory medicines like aspirin to manage flares. Patient can also do certain things to help manage their lupus, such as stopping smoking and avoiding sunlight.
A Conversation With a Lupus Patient
Here is part of an interview with a 12 year old lupus patient (Miah) and her mom (Elizabeth).
Warda (Interviewer): When did you know something was wrong?
Elizabeth (Mom): Miah had pits on her fingernails. A year later we noticed the same symptom on her toenails, then a rash appeared on the side of her lip and nose. I decided to visit a dermatologist who prescribed an antibiotic and cream for Miah’s rash. That did not help her clear the rash, so we visited another dermatologist.
Miah (Lupus warrior): I knew something was wrong when I visited many different dermatologists and the rash would not disappear. My rash started to expand.
Warda: When and how did you find out that Miah had lupus?
Elizabeth: It took 2 years to finally get a diagnosis for Miah. They did a lot of blood work, and it all came back normal. She did have protein in her urine, but the physician believed it was due to dehydration. The dermatologist we met with decided to take a skin sample for testing, and that was very scary for me to see because the sample they took was quite large. Finally, the dermatologist confirmed a diagnosis of lupus. The rheumatologist confirmed that Miah’s rash, nail bed pitting, mouth ulcers, and the protein in her urine were due to her lupus.
Warda: What are some of the biggest challenges of living with a chronic disease?
Miah: In the beginning, it was very overwhelming. I have learned that I cannot be in the heat or humidity because it makes my symptoms worse, and it causes extreme fatigue. During my middle school graduation, I was outside under the shade of a tree, but the heat was still too much. My mom had to pick me up and I was physically in so much pain. Now, I have a backpack that carries cooling sleeves, a hat, and a scarf to keep me protected when I am in the heat. I also used to do karate but because of my joint pain, I am no longer able to do that. My rheumatologist recommended physical therapy to strengthen my knee muscles. As part of my 504 plan, I am going to be taking dance classes during high school, instead of gym, to avoid any outdoor exposure.
Warda: What advice would you give to others battling lupus?
Miah: It is going to be challenging in the beginning, but it will get better. It is important to figure out what you should be doing, such as eating anti-inflammatory foods or staying out of the sun. The most important piece of advice is: listen to your body.
Elizabeth: It is important to educate yourself about lupus and to advocate for your child. Also, do not rely on blood work to give you the diagnosis because that will not always be sufficient. In school, when advocating for your child, make sure to set up a 504 educational plan. That is a legal document that, in the United States, provides accommodations and support to students with disabilities, to ensure equal access to education. For instance, under the 504 plan, were able to get air conditioning in Miah’s school to help her avoid heat exhaustion.
Summary
In summary, lupus is a condition where the body’s defense system mistakenly attacks its own cells. This can lead to a wide range of health issues. Fortunately, there are ways to manage it. Doctors have tests and treatments that can help people with lupus feel better. Think of your body’s defense system as a superhero team. Sometimes, they get a little mixed up and start fighting the wrong battles. That is what happens in lupus. But here is the inspiring part: people dealing with lupus, like Miah, are the real fighters. Miah has taken the necessary steps to educate herself on lupus and has learned to manage it. With the right help and knowledge, living with lupus can become a bit easier.
Glossary
Immune System: ↑ A team of cells and proteins fighting germs. Protects you from getting sick and helps you get better.
Autoimmune Disease: ↑ Occurs when the immune system confuses our own body healthy cells as enemies, triggering attacks.
B Cells: ↑ A type of white blood cell that is responsible for producing antibodies that identify, tag, and neutralize harmful pathogens like bacteria or viruses.
Antibodies: ↑ These are proteins made by the immune system to identify and neutralize harmful invaders like viruses or bacteria, helping the body fight infections and stay healthy.
Immune Complexes: ↑ Clumps formed when antibodies and cellular debris stick together, signaling the immune system to remove them, which causes an inflammatory response.
Inflammatory Response: ↑ This is the body’s defense mechanism against harmful things like infections or injuries. It involves redness, swelling, and heat as the body’s way of fighting and healing.
Autoantibodies: ↑ Antibodies that mistakenly attack the body’s own cells instead of protecting them.
Nephritis: ↑ This is kidney inflammation, often from infections or autoimmune issues. It leads to symptoms like blood in urine, swelling, and high blood pressure, impacting kidney function and health.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Charras, A., Smith, E., and Hedrich, C. M. 2021. Systemic lupus erythematosus in children and young people. Curr. Rheumatol. Rep. 23:20. doi: 10.1007/s11926-021-00985-0
[2] ↑ Barbhaiya, M., and Costenbader, K. H. 2016. Environmental exposures and the development of systemic lupus erythematosus. Curr. Opin. Rheumatol. 28:497–505. doi: 10.1097/BOR.0000000000000318
[3] ↑ Diaz-Frias, J., and Badri, T. 2022. Neonatal lupus erythematosus. In StatPearls. St. Petersburg, FL: StatPearls Publishing..
[4] ↑ Cojocaru, M., Cojocaru, I. M., Silosi, I., and Vrabie, C. D. 2011. Manifestations of systemic lupus erythematosus. Maedica 6:330–6.
[5] ↑ Dörner T. 2010. Therapy: hydroxychloroquine in SLE: old drug, new perspectives. Nat. Rev. Rheumatol. 6:10–11. doi: 10.1038/nrrheum.2009.235