Abstract
Have you ever seen a small baby with yellow skin or eyes? These babies have a skin condition called jaundice and it is actually pretty common. Jaundice occurs when too much of a waste substance called bilirubin stays in the blood for too long. Bilirubin is produced when red blood cells naturally break down and, in high amounts, it can cause damage to the body. The most common way doctors identify jaundice is the finger test: gently touching the baby’s skin with their finger to look for any yellowing. If the baby does have jaundice, there are two main treatments: ultraviolet (UV) light therapy and exchange transfusion therapy. Both work by bringing bilirubin in the blood down to normal levels.
What Is Neonatal Jaundice?
Neonatal jaundice is a common condition experienced by about 60% of all babies [1]. “Neonatal” is a word that doctors use to refer to newborn babies. So, what is jaundice? Jaundice is a condition that turns the skin yellowish, due to high levels of a waste substance called bilirubin in the blood. Neonatal jaundice, or high bilirubin levels in newborns, is one of the main reasons why babies stay in the hospital during their first week of life. Because jaundice is so common, you or one of your friends may have had jaundice as a baby. Some babies are at higher risk of developing jaundice, such as those born earlier or later than the normal 40 weeks [1]. If left untreated, severe jaundice can lead to vision problems and even brain damage [1]. Thus, parents and healthcare professionals should take jaundice seriously, and make sure to follow the recommended steps to treat it. Since jaundice is so common, this article may help you understand why a baby you know had to stay in the hospital to receive treatment for a while after being born. Who knows? Maybe after reading this paper, you could even help identify the signs of undiagnosed jaundice in a baby, and tell their parent or caregiver that the baby should be seen by a doctor.
Where Does Jaundice Take Place In The Body?
Now that you know a little bit more about what jaundice is and why it matters, you may be wondering how it happens and what parts of the body are involved in this condition. To answer these questions, we must dive into the function of the liver, and the important it plays in keeping us healthy.
We will start by talking about bilirubin, because it is abnormal levels of this substance that lead to jaundice. What exactly is bilirubin? Bilirubin is a red/orange-colored compound that is created when hemoglobin (an important part of red blood cells) naturally breaks down. Bilirubin travels to the liver, where it is eventually released as waste [2]. Interestingly, newborns have much more bilirubin in their blood than adults do, because their red blood cells break down more than those of adults [1]. Normally, the liver does a good job of removing bilirubin and other wastes from the blood. With jaundice, however, the liver has a hard time functioning, which leads to too much bilirubin staying in the blood (Figure 1) [2].
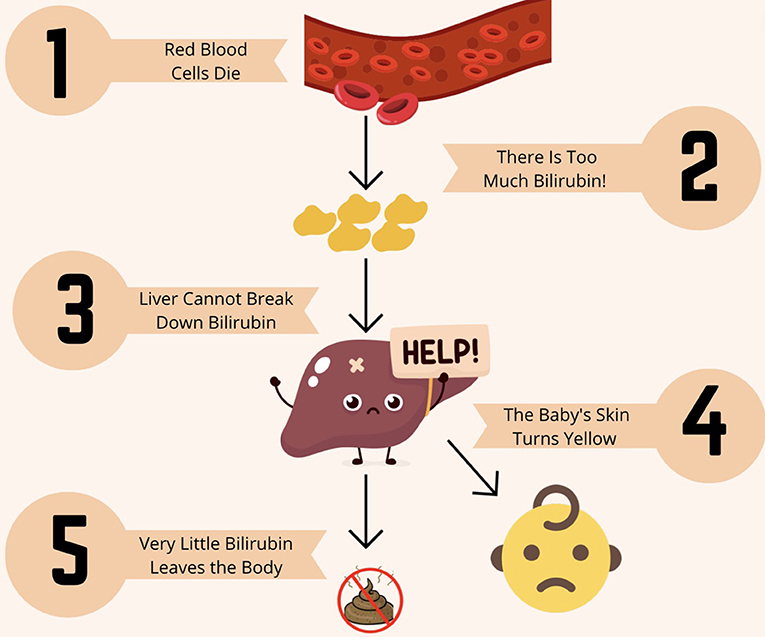
- Figure 1 - Normally, when red blood cells die, the liver breaks down bilirubin so it can leave the body in our poop.
- In newborns, red blood cells die more quickly than in adults, which leads to higher levels of bilirubin than the liver is able break down. When less bilirubin is broken down and leaves the body in our poop it builds up causing yellowing of the skin.
The medical term for jaundice is hyperbilirubinemia. We can break down this word to better understand it. The first part, “hyper,” means “too much.” The middle part, “bilirubin,” is the substance that is produced when hemoglobin breaks down. The last part, “emia,” refers to the fact that the bilirubin is found in the blood. When we put it all together, “hyperbilirubinemia” means too much of the substance called bilirubin in the blood. This causes the skin to turn yellow [2].
How Do We Know A Baby Has Jaundice?
How do we know a baby has jaundice? Neonatal jaundice can appear as early as the first or second day of a baby’s life. The baby’s face slowly starts to turn yellow, along with the whites of the eyes. The yellow color eventually makes its way down the body to the legs [1].
You may think the yellow color makes jaundice easy to diagnose, but it can actually be difficult to identify at first. Most babies look a little yellow when they are only a few days old, and that is considered normal [1]. Also, darker skin complexions can hide the yellow color from jaundice [1]. However, there is an easy way to look for jaundice, which we will call the finger method. Using a finger, doctors can press down on a baby’s skin, and if the skin turns yellow after the finger is removed, the baby likely has jaundice [1].
Laboratory tests can also diagnose jaundice. There are special tools to measure bilirubin, which are called bilirubinometers. One type is called a transcutaneous bilirubinometer, and it is a medical device that measures bilirubin levels through the skin. Transcutaneous bilirubinometers work by shining a bright light on the baby’s skin and measuring the light that is reflected back. Since light is either reflected or absorbed, we know that any light not reflected back to the machine has been absorbed by bilirubin in the baby’s skin. The machine measures the light that is reflected vs. absorbed and uses this information to calculate the amount of bilirubin present [3]. Transcutaneous bilirubinometers are great because they work through the skin and do not cause the baby any pain. Another method for measuring bilirubin requires the baby to have a small amount of blood drawn, so that bilirubin levels can be measured directly. This method is used when the baby develops jaundice within 24 h of birth, or if the transcutaneous bilirubin readings are very high [1].
How Do Doctors Treat Jaundice?
Doctors help babies fight jaundice through special treatments. Treatments are needed when bilirubin levels are high, because high levels can affect the rest of the body. Doctors can use two main treatments: ultraviolet phototherapy and exchange transfusion therapy [1].
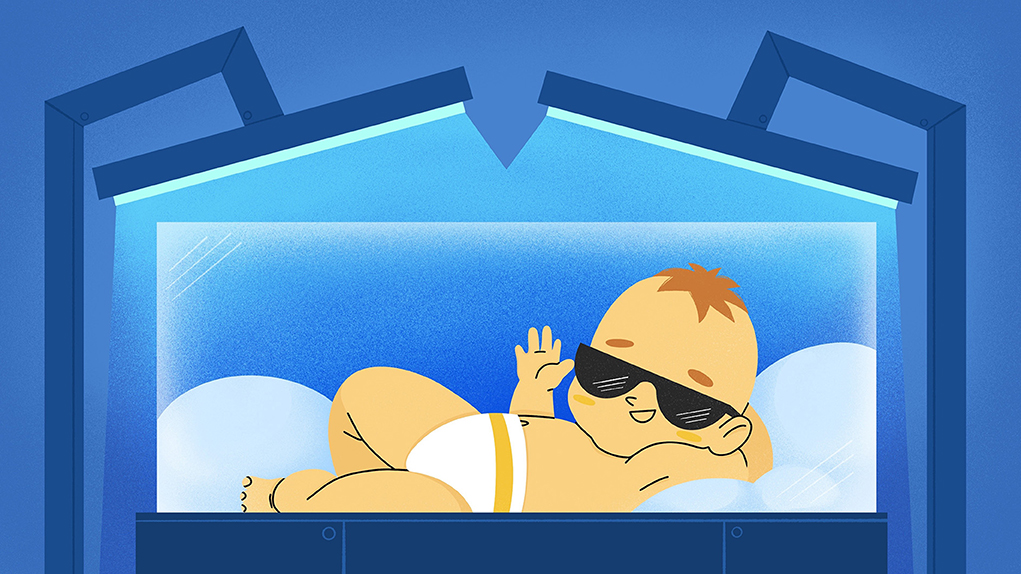
Imagine a baby in a blue box, wearing sunglasses. The baby is actually receiving treatment for jaundice through ultraviolet (UV) phototherapy (Figure 2) [4]. In UV phototherapy, the baby is placed in an incubator under a blue light. The baby’s eyes are covered so that the UV light does not damage them. The baby is flipped over every few minutes, so that most of the skin is well exposed to the treatment [4]. When the blue light hits the baby’s skin, bilirubin absorbs light molecules. Then, fast reactions occur that turn bilirubin into other substances that are not harmful and can leave the baby’s body in the poop [5, 6]. The baby receives this treatment throughout the day, with short 30-min breaks so that the baby can eat. Bilirubin levels are continuously checked until doctors are sure that the levels are normal [7].
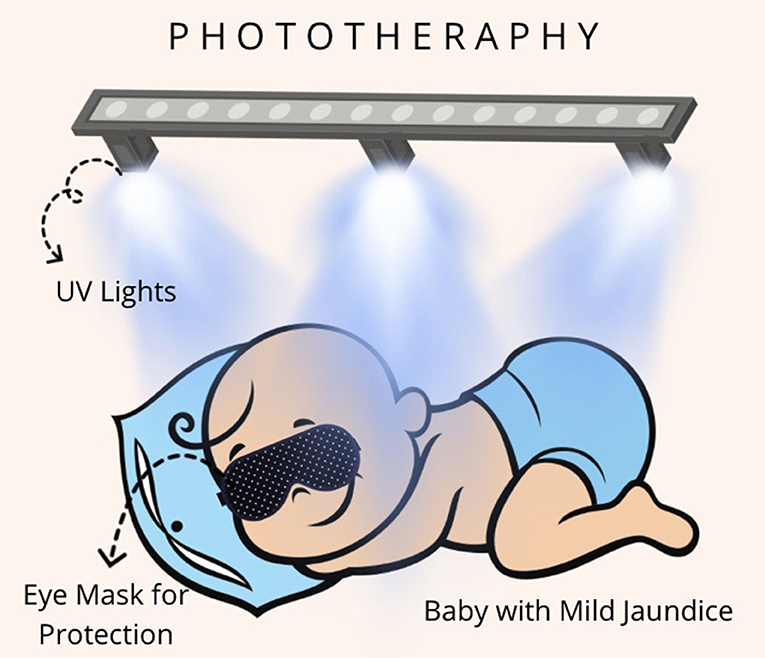
- Figure 2 - One way to treat neonatal jaundice is to use UV phototherapy.
- In this therapy, the baby’s skin is exposed to a UV light. The bilirubin in the blood absorbs light molecules which causes it to break down into substances that can leave the body in our poop. To get the best results, the baby is turned over so as much of their skin is exposed to the light as possible. Since UV light is harmful to our eyes, the baby wears a mask similar to sunglasses.
The baby receives a low level of UV light, which is considered safe, but may cause some dehydration, skin rashes, and overheating. This is why babies need to be monitored during UV phototherapy to ensure there are no signs of harm and to address issues if they do arise. For example, babies could be given liquids if they are getting dehydrated, or a doctor or nurse might apply some cream if babies get a rash. Once bilirubin levels are back to normal, the UV phototherapy is stopped, and the baby is moved out of the incubator.
Sometimes the bilirubin level is so high that UV phototherapy cannot lower it to safe levels. The baby might need exchange transfusion therapy. In this therapy, the baby is connected via a blood vessel in their arm, leg, or umbilical cord to a thin tube that swaps the baby’s blood for new blood [1]. This process takes a few hours. After the treatment, the nurse or doctor checks the baby’s bilirubin levels again. If bilirubin levels are still too high, the baby will receive the therapy again. If the levels are normal, then the tube will be removed. Doctors know the treatment works when the yellow skin color goes away, and a blood test shows normal bilirubin levels. So, if you ever see a baby in a blue light box or connected to tubes, they might be getting treatment for jaundice.
Conclusion
By reading this article, you learned that jaundice is a common and important condition that affects many newborns and needs to be treated [2]. Since babies break down red blood cells faster than adults do, jaundice is both more common and easier to treat in babies than in adults. Adults can get jaundice too, but this is most often because there is something wrong, such as liver damage or blockage. This means that treating jaundice in adults is more challenging.
It is important that neonatal jaundice be identified and treated early. If bilirubin levels keep rising, it can lead to severe conditions that disrupt the baby’s brain, eyesight, and teeth [1]. By learning more about how jaundice develops, its symptoms, and how doctors treat it, you now have a better understanding of how skin color gives doctors a hint about our health. Now you can understand why some babies need to spend time inside UV phototherapy boxes… and maybe one day, you will notice a baby with yellow skin and ask an adult if the baby has been seen by a doctor to determine if it has jaundice!
Glossary
Jaundice: ↑ Condition in which a person’s skin yellows because of too much bilirubin (red/orange-colored compound) in their blood, indicating that the liver cannot properly break down hemoglobin from red blood cells.
Neonatal: ↑ A word to describe newly born babies or children under 28 days old.
Bilirubin: ↑ A red/orange colored substance that is created when red blood cells break down and can build up in the skin, causing a yellowish color.
Hyperbilirubinemia: ↑ A medical term for jaundice that uses Latin word roots to say there is too much (hyper-) bilirubin in the blood (-emia).
Transcutaneous Bilirubinometer: ↑ A device that determines bilirubin levels in the blood by shining a light through the skin and measuring how much light is reflected back, instead of being absorbed by bilirubin.
Ultraviolet Phototherapy: ↑ A special type of light therapy that is used to treat jaundice, in which a color of light called ultraviolet is shone on the baby.
Exchange Transfusion Therapy: ↑ An alternative to UV phototherapy, in which babies’ blood is replaced with bilirubin-free blood to treat jaundice.
Umbilical Cord: ↑ A tube connecting the mother to their baby, which serves to transfer nutrients to the baby and help it grow.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ National Collaborating Centre for Women's and Children’s Health. 2010. Neonatal Jaundice. London: RCOG Press. Available online at: https://www.ncbi.nlm.nih.gov/books/NBK65119/ (accessed May 13, 2023).
[2] ↑ National Library of Medicine. 2023. Jaundice. Stat Pearls. Available online at: https://www.ncbi.nlm.nih.gov/books/NBK544252/ (accessed February 21, 2023).
[3] ↑ Okwundu, C. I., Olowoyeye, A., Uthman, O. A., Smith, J., Wiysonge, C. S., Bhutani, V. K., et al. 2017. Transcutaneous bilirubinometry versus total serum bilirubin measurement for newborns. Cochrane Database Syst. Rev. 5:CD012660. doi: 10.1002/14651858.CD012660.pub2
[4] ↑ Csoma, Z., Kemeny, L., and Olah, J. 2008. Phototherapy for neonatal jaundice. New Engl. J. Med. 358:2523–4.
[5] ↑ Wang, J., Guo, G., Li, A., Cai, W. Q., and Wang, X. 2021. Challenges of phototherapy for neonatal hyperbilirubinemia (Review). Exp. Ther. Med. 21:231. doi: 10.3892/etm.2021.9662
[6] ↑ Stokowski, L. A. 2006. Fundamentals of phototherapy for neonatal jaundice. Adv. Neonatal Care 6:303–12. doi: 10.1016/j.adnc.2006.08.004
[7] ↑ Wong, R., and Bhutani, V. 2022. Patient Education: Jaundice in Newborn Infants (Beyond the Basics)—UpToDate. Available online at: https://www.uptodate.com/contents/jaundice-in-newborn-infants-beyond-the-basics/print (accessed January 13, 2024).