Abstract
Within their small air sacs, our lungs exchange oxygen (O2) from the air for the carbon dioxide (CO2) produced by our bodies. In these air spaces, O2 moves into small blood vessels while CO2 moves from the blood out into the air. Lung diseases can impair airflow and reduce the number of blood vessels in the lungs, making it harder to take in O2 and eliminate CO2. These changes to the lungs contribute to symptoms like breathlessness. The relationship between airflow and blood flow in our lungs is called V/Q, where V is for ventilation—the movement of air—and Q is for perfusion—blood flow to the lungs. While people with healthy lungs have good a good match between V and Q, those with certain lung diseases often have poor V/Q matching. In this article, we describe the origins of V/Q mismatch and its impact on lung function.
Lungs: The Basics
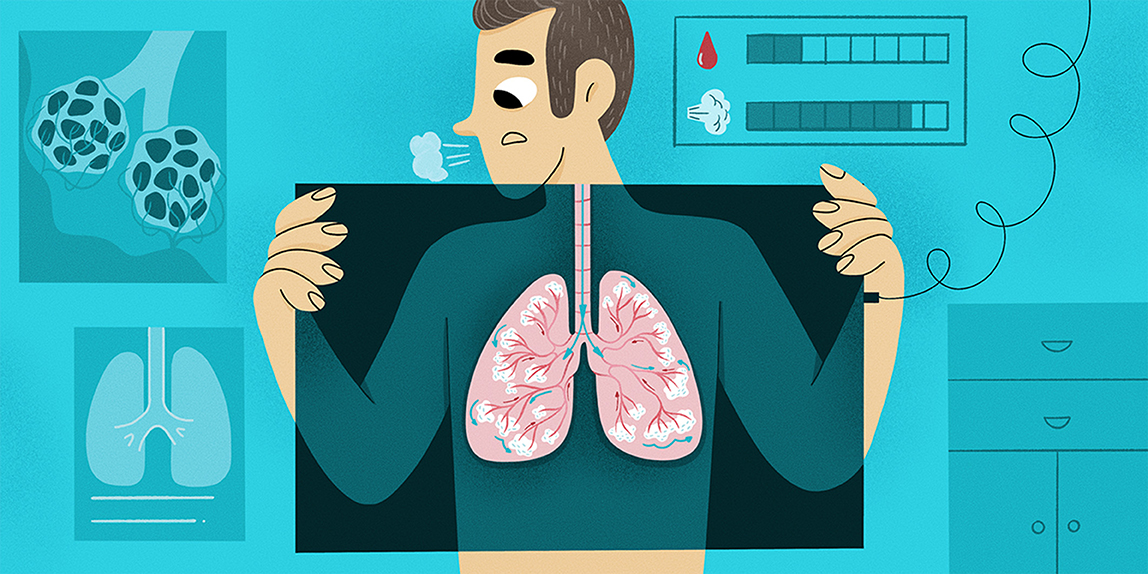
Much like an inflating balloon, our lungs expand when we breathe in because of the contraction of a large muscle called the diaphragm. When the diaphragm relaxes, the air leaves the lungs, allowing them to return to their resting size. However, one important difference between a balloon and the lungs is that the air that enters our lungs when we breathe in is not the same as the air that leaves our lungs when we breathe out. The lungs perform two important tasks. First, they allow us to take oxygen (O2) from the air we breathe into the bloodstream, so we can use it to produce energy and survive. Second, they remove the carbon dioxide (CO2) waste that our cells produce, returning it back out into the air. In other words, the small air sacs within our lungs, called alveoli, exchange O2 from the air with CO2 found within the small lung blood vessels, called pulmonary capillaries (Figure 1). This process is called gas exchange.

- Figure 1 - Gas exchange.
- When the diaphragm contracts and relaxes, air enters and exits our lungs through airways: the trachea and bronchi. These airways become smaller and smaller as they travel from the mouth down into the lungs: they branch 23 times before the air reaches the smallest functional unit of the lungs, the alveoli. Alveoli are small sacs of air where gas exchange (O2 for CO2) occurs. The alveoli are found very close to tiny blood vessels called pulmonary capillaries, because blood is needed for gas exchange to happen.
Gas exchange is the most important function of the lungs. It depends on both a sufficient air supply and a good blood supply to work properly. Blood that contains more oxygen is bright red in color, whereas blood with less oxygen has a more blueish color. In diagrams, the blood color is therefore often shown as either blue (when there is low O2 and high CO2) or red (when there is high O2 and low CO2).
What Is Dead Space?
Dead space is the name for the regions of the lungs that do not exchange gases. There are two main types of dead space: anatomic dead space and alveolar dead space. Everyone, including people with healthy lungs, has anatomic dead space. An example of anatomic dead space is the trachea, the large airway that connects the mouth and nose to the lungs. The trachea (a.k.a. windpipe) has sturdy walls that are too thick to allow gases to pass through them into any blood vessels in the area. Thus, while air moves through the trachea on its way to the alveoli, CO2, and O2 are not exchanged! The size of each person’s anatomic dead space relates to the size of their airways and body. One extreme example seen in nature is the giraffe. Because of their very long necks, giraffes have much more anatomic dead space than humans do.
Alveolar dead space refers to any parts of the lungs that do not receive sufficient blood flow. You will recall that gas exchange depends on air being near the blood in the pulmonary capillaries. If there is no blood, there is nowhere for the O2 in the air to go: the air in these alveoli has essentially been wasted! This is what happens in areas of alveolar dead space. V/Q mismatch is the scientific name for when alveolar dead space is created because something is wrong with gas exchange. The fresh air (V, for ventilation) in the lungs is not being appropriately matched by the blood flowing to the lungs (Q, for perfusion). V/Q mismatch can be measured by imaging the air and blood in the lungs, or by analyzing the gases coming out of the lungs. Whatever the cause of the V/Q mismatch, poor gas exchange can cause health problems (Figure 2).
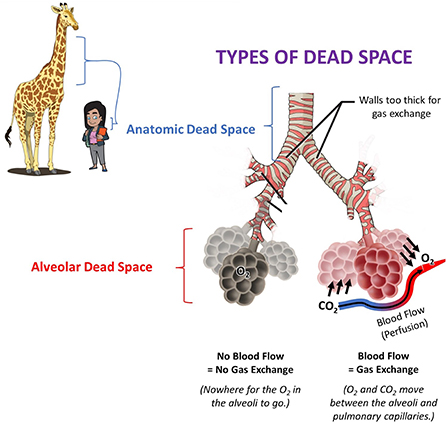
- Figure 2 - Anatomic dead space includes parts of the respiratory system where gas exchange cannot occur, such as the trachea.
- Giraffes have very long necks and tracheas, and therefore have more anatomic dead space than humans do. Alveolar dead space involves alveoli that do not have healthy blood vessels nearby. Without both functional air and blood supplies, gas exchange cannot occur. Blood is needed to both eliminate the waste product CO2 into the air and to collect the O2 that we take in from the air.
What Is Obstructive Lung Disease?
Obstructive lung disease is the name for a group of lung diseases that have one thing in common: damage to the airways that makes it harder to breathe air in and out of the lungs. Sometimes small muscles within the airways contract, squeezing the airways until they are very narrow and making it hard for air to pass. This is often the case in conditions like asthma. Other times, the lungs, alveoli, and airways become damaged, weak, and floppy, making it hard for the airways to stay open and causing air to get trapped in some of the alveoli. This is the case in chronic obstructive pulmonary disease (COPD) [1], which is a common type of obstructive lung disease very strongly linked with smoking. While being exposed to things like smoke from cigarettes or cooking fires are known risk factors for developing COPD, the likelihood of developing certain lung diseases can also be passed down within families. This is the case for some people with COPD, who are more likely to develop COPD when exposed to similar types of risk factors as compared with other individuals.
Other obstructive diseases like asthma and allergies can be directly triggered by things in the environment, like pollen, dust, or cold temperatures. It is important to study obstructive lung disease because about one out of every seven people [2] has some form of obstructive lung condition—and that number is expected to increase as air pollution all over the world makes lung disease more likely. While obstructive lung disease makes it difficult to get air in and out of the lungs, it is important to realize that it affects more than just the airways. This is especially true for COPD.
How Does V/Q Mismatch Make Obstructive Lung Disease Worse?
Remember that both air supply and blood supply are necessary for gas exchange. Imagine if the air supply was blocked (i.e., obstructed), like someone pinching closed the opening of a balloon. Gas exchange cannot occur under these conditions because no O2-containing fresh air can get into the alveoli, and the CO2 delivered to that region of the lung by the pulmonary capillaries cannot get out. The obstruction of airways that occurs in obstructive lung disease therefore decreases ventilation. This impacts one part of the V/Q relationship—ventilation.
However, even in cases where there is sufficient air supply, gas exchange can be disrupted if there is not enough blood supply to the pulmonary capillaries. Research shows that patients with COPD have less blood flowing to their lungs than do people of a similar age who have healthy lungs [3, 4]. Since there is less blood supply going to the lungs, parts of the lungs are not being perfused. This impacts the perfusion part of the V/Q relationship. In COPD, therefore, both ventilation (V) and perfusion (Q) are altered, leading to V/Q mismatch and a higher-than-normal alveolar dead space. Patients with COPD therefore often do not get enough O2 and can sometimes have elevated levels of CO2. This V/Q mismatch and the resulting alterations in blood gases contribute to the symptom of breathlessness that patients with COPD often experience. To truly help improve lung function in people with COPD, we should try to improve both air supply and blood flow.
Can We Improve V/Q Mismatch?
How can we help people with obstructive lung disease exchange gases properly again? The current gold standard for treatment involves drugs called bronchodilators (“broncho-” = airway; “dilation” = to make larger). Bronchodilators relax the airways, making them more open so it is easier to move air in and out of the lungs (Figure 3). This helps O2 to be delivered to the alveoli more easily, where it can enter the blood in the pulmonary capillaries. In cases where bronchodilator treatment is not enough, an additional treatment option is to provide the patient with air that contains much more O2 than is normally found in the air around us. This treatment, which is called supplemental O2 therapy, helps force O2 into the blood even when airflow and blood flow are lower than normal [5].
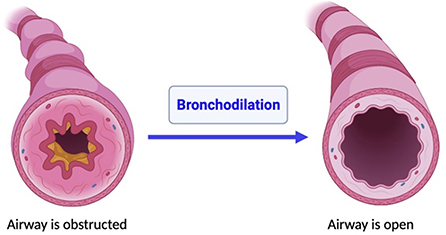
- Figure 3 - Bronchodilation.
- When the muscles that make up airway walls dilate (i.e., relax or expand), it makes the airways become larger inside. This allows air to travel through the airways more easily. The left panel shows a cross-section of an obstructed airway with a small airway opening. The right panel shows how the airway expands after bronchodilator treatment, resulting in a larger airway opening.
Bronchodilators and supplemental O2 therapy both only target the delivery of air, though. They do not change the blood flow to the lungs. New and emerging research using substances that can improve blood flow, such as nitric oxide [6], may help to determine whether certain individuals benefit from changes to their blood flow as well as their airflow. Nitric oxide is normally produced in very small amounts by the body. It causes blood vessels to relax and be more open, allowing more blood to flow through them. If a medication could have a similar effect in the lungs, this might help improve blood flow in those people where blood flow to the lungs is decreased. Exciting new research is trying to identify what individuals are most likely to benefit from treatments that may one day include medications to improve blood flow! Overall, the goal of any of these treatments is to help restore the V/Q balance, improving gas exchange and symptoms in patients with a high amount of alveolar dead space.
Conclusion
In summary, gas exchange is the most important function of the lungs and requires both blood flow and airflow. Gas exchange is impaired in patients with COPD. For many years, treatments for COPD have focused on opening the airways; however, this ignores emerging knowledge that there are also problems with blood flow that can worsen V/Q mismatch. Ongoing research is investigating whether it might also be important to improve blood flow in the treatment of COPD. Looking forward, researchers hope to create treatment strategies to best improve gas exchange, and therefore improve symptoms and quality of life, in each unique individual.
Glossary
Alveoli: ↑ The smallest units of the lungs; very small, sac-like airspaces that are the primary site of gas exchange.
Pulmonary Capillaries: ↑ The smallest blood vessels in the lungs; these have very thin walls to allow O2 and CO2 to be exchanged between the blood and air.
Gas Exchange: ↑ The transfer of oxygen (O2) into our bodies and carbon dioxide (CO2) out of our bodies; this process occurs in our lungs where air spaces and small blood vessels meet.
Dead Space: ↑ Regions of the lungs that do not perform gas exchange. Total dead space is made up of both anatomic and alveolar dead space.
V/Q Mismatch: ↑ When the ventilation (V) to an area of the lung is relatively too high or too low for the level of perfusion (Q) to that area of the lung.
Ventilation: ↑ The amount of air that moves in and out of the body per minute; it is represented by “V” in the expression V/Q mismatch.
Perfusion: ↑ The volume of blood that moves through specific tissues in a certain amount of time; it is represented by “Q” in the expression V/Q mismatch.
Obstructive Lung Disease: ↑ Diseases that involve damage to the airways, so that it is harder to move air between the environment and lungs; this includes asthma and Chronic Obstructive Pulmonary Disease.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
Figures were created using Power Point and images publicly available through Creative Commons.
Abbreviations
CO2, Carbon dioxide; COPD, Chronic Obstructive Pulmonary Disease; O2, Oxygen; V/Q, ventilation and perfusion.
References
[1] ↑ Poor, H. D., Kawut, S. M., Liu, C.-Y., Smith, B. M., Hoffman, E. A., Lima, J. A., et al. 2005. Pulmonary hyperinflation due to gas trapping and pulmonary artery size: the MESA COPD study. PLoS ONE. 12:e0176812. doi: 10.1371/journal.pone.0176812
[2] ↑ Murtagh, E., Heaney, L., Gingles, J., Shepherd, R., Kee, F., Patterson, C., et al. 2005. The prevalence of obstructive lung disease in a general population sample: the NICECOPD study. Eur. J. Epidemiol. 20:443–53. doi: 10.1007/s10654-005-1248-8
[3] ↑ Wagner, P. D., Dantzker, D. R., Dueck, R., Clausen, J. L., and West, J. B. 1977. Ventilation-perfusion inequality in chronic obstructive pulmonary disease. J. Clin. Invest. 59:203–16. doi: 10.1172/JCI108630
[4] ↑ Hueper, K., Vogel-Claussen, J., Parikh, M. A., Austin, J. H., Bluemke, D. A., Carr, J., et al. 2015. Pulmonary microvascular blood flow in mild chronic obstructive pulmonary disease and emphysema. The MESA COPD study. Am. J. Respir. Crit. Care Med. 192:570–80. doi: 10.1164/rccm.201411-2120OC
[5] ↑ Eaton, T., Fergusson, W., Kolbe, J., Lewis, C., and West, T. 2006. Short-burst oxygen therapy for COPD patients: a 6-month randomised controlled study. Euro. Respir. J. 27:697–704. doi: 10.1183/09031936.06.00098805
[6] ↑ Ashutosh, K., Phadke, K., Jackson, J., Steele, D. 2000. Use of nitric oxide inhalation in chronic obstructive pulmonary disease. Thorax. 55:109–13. doi: 10.1136/thorax.55.2.109