Abstract
Did you know Alzheimer’s disease (AD) is a worldwide leading cause of disability and death in later life? Patients with AD usually can not recognize their own families or take care of themselves. Often called “the long goodbye,” AD is a heartbreaking struggle for both patients and their caretakers. For a long time, doctors were helpless in treating AD patients. Even now, there is no cure for AD. But fortunately, brain scanning techniques have recently advanced enough to help AD patients a great deal. These techniques are ways for doctors to see the inner workings of the living patient’s brain, without surgery. Thus, brain imaging techniques are valuable tools that can help doctors catch AD early, provide customized care for each patient over the course of the disease, and guide future research toward finding a cure. Thanks to these developments, the prospects for AD patients are slowly but steadily improving.
Importance of Peeking Inside the Living Brain
Did you know that the first brain scan was performed in 1927 by Tan and Yip [1]? He had no idea of the impact his work would have on healthcare. Nowadays, doctors routinely rely on brain scans, also called neuroimaging, to diagnose and treat patients. Neuroimaging allows doctors to observe the inner workings of a patient’s brain without having to open the skull using surgery. It also allows doctors to catch various problems much earlier than they would by simply observing the patient’s outward behavior. Doctors use various imaging techniques to take pictures of the brain. They then use these scans to reliably diagnose diseases that cause the wasting away of brain tissue, called neurodegenerative diseases. There are several kinds of neurodegenerative diseases, including Parkinson’s disease, multiple sclerosis, and Huntington’s disease. Although we will focus on Alzheimer’s disease (AD) in this article, neuroimaging can greatly help patients with other neurodegenerative diseases as well.
Alzheimer’s Disease Is Difficult To Diagnose
AD is named after Dr. Alois Alzheimer, who first described it in 1906. It is a common form of dementia. AD typically affects adults aged 65 and older, although early-onset AD can start between 40 and 50 years old. Every year, about 30 million people are diagnosed with AD worldwide, and about 2 million people die from AD-related causes. However, the cause of AD is still unknown. AD is characterized by shrinking of the brain, including the hippocampus, a brain region that plays a key role in memory formation, memory storage, and learning. As AD progresses through mild, moderate, and severe stages, brain shrinkage and the patient’s signs and symptoms worsen (Figure 1). There is currently no cure for AD; all doctors can do is reduce the patient’s suffering.
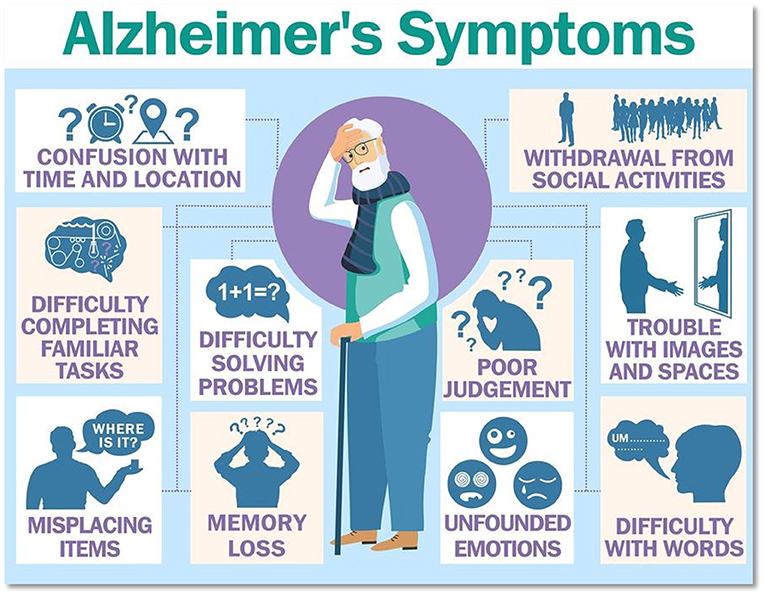
- Figure 1 - Symptoms of AD.
- The disease is accompanied by a variety of symptoms that impact the way the patients live their lives. Notice how similar these AD symptoms are to the signs of normal aging. Based on these outward symptoms alone, would you be able to tell an AD patient apart from a healthy person of the same age? (Image credit: https://www.askdrray.com/a-new-drug-for-alzheimers/).
During the mild stage of AD, patients can take care of themselves but experience worsening memory loss and declining mental abilities, such as trouble recalling names or words, forgetting things they have just read, and misplacing things. The more noticeable symptoms during this stage are intense mood swings, confusion, disorientation, slowed speech, and trouble planning and organizing things. People in the mild stage may show poor judgement and decision-making skills. Concentration declines and attention span shortens; the patient’s personality may begin to change as well. Notice how these symptoms are so similar to signs of normal aging. This makes AD difficult to diagnose during the initial stages of the disease.
The moderate stage is the longest. Symptoms are now more noticeable, and the patient’s personality and behaviors begin to change even more. Memory loss worsens as the patient forgets major details, like the names and purposes of objects. During this stage, patients become mistrustful of family and friends and withdraw from them. They also show signs of depression and anxiety, alongside frequent mood swings. Sleep patterns become unusual; they sleep during the day but are restless at night. Patients have an increased tendency to wander and get lost or disoriented. During this stage, the patient likely cannot continue a job and needs a full-time caretaker.
During the final and most severe stage of AD, patients show severe memory loss; many patients forget their loved ones. Patients can no longer interpret what they are seeing or hearing. They may not understand what is said to them, and they struggle to string sentences together or speak at all. At this point, the brain damage interferes with the ability of patients to control their bodies, so patients require walkers, wheelchairs, or assistance from caretakers. Patients also become more susceptible to infections. It is common for AD patients to die of infection rather than AD itself [2].
Pet: Tracing Changes in the Brain
Fortunately, neuroimaging techniques can help with diagnosis of diseases like AD, by allowing doctors to look inside the brain. One such technique is called positron emission tomography (PET). PET is a technique in which the patient is given a relatively safe radioactive substance called a tracer that tracks the chemical changes happening in the target body region, which, in this case, is the brain. A common tracer tracks the absorption of glucose by various bodily tissues [3]. Lower levels of glucose absorption in the brain can indicate AD (Figure 2A). However, the glucose tracer alone is usually not enough to diagnose AD, because it cannot distinguish AD from other diseases that affect glucose uptake in the brain, including other types of dementia. Therefore, along with the tracer for glucose absorption, it is important for doctors to use other types of PET tracers that also tag signs of AD [2, 3].
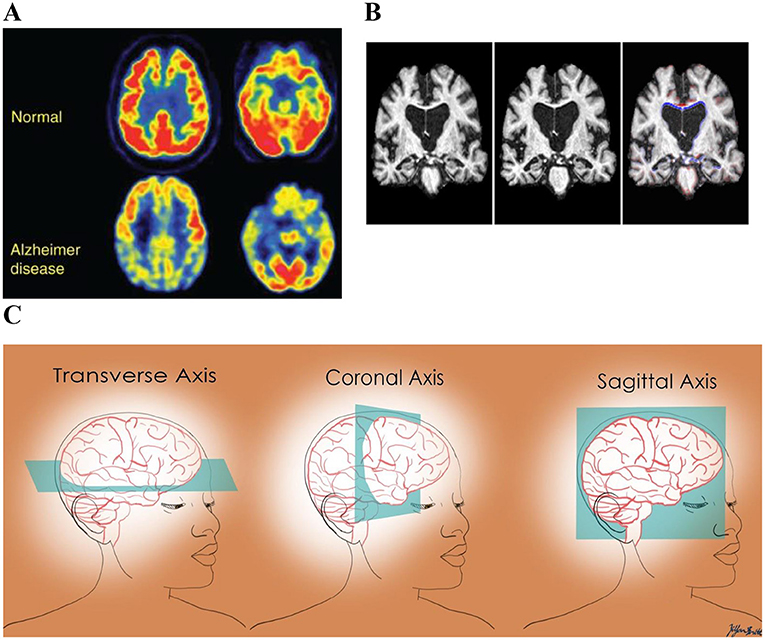
- Figure 2 - (A) A PET tracer is used to show the high metabolic activity (red) that is typical for a normal brain.
- Low levels of brain activity (blue) are seen in the brains of AD patients [4]. (B) MRI can show brain shrinkage. The left image is a scan taken when a patient was first diagnosed with AD. The middle image was taken 2 years later. The right image shows both images overlapped, with blue indicating where the brain shrank. (C) Neuroimaging allows doctors to examine the brain from different angles, such as the ones shown here, to see which specific brain regions are affected by disease or injury [Image credits: (A) see [3]; (B) https://www.nature.com/articles/s41598-018-29295-9; (C) ZiYan Britt].
PET is very useful in diagnosing neurodegenerative diseases because it allows the doctor to observe changes in cells, even when there is no apparent effect on the patient’s behavior. Thus, PET can help doctors identify signs of AD before the symptoms become severe. Early diagnosis of AD is one of the reasons doctors use neuroimaging to observe the brain. However, PET is not very good at helping us understand AD.
MRI: The Big Magnet That Can See Through the Skull
More recently, another brain imaging technique was developed and continues to be a popular diagnostic tool today: magnetic resonance imaging (MRI). MRI uses powerful magnetic fields to create detailed 3D images of the brain. For more information on how MRI works, please see this Frontiers for Young Minds article [4]. The different levels of brightness in the MRI image help doctors determine the identity and health of a tissue (Figure 2B). MRI images can show “slices” of the brain from almost any viewpoint (Figure 2C) [5]. Doctors study these MRI “slices” to spot any abnormalities that suggest a disease or disorder.
One of the abnormalities that MRI measures far more effectively than PET is a shrinking of the brain. For instance, MRI shows brain shrinkage in the hippocampus, which is a characteristic of AD. When symptoms are still mild, MRI usually shows that the size of the hippocampus is 15–25% smaller in AD patients compared to healthy people [3]. Thus, using MRI, doctors can observe the extent of AD in the brain, instead of just relying on the patient’s behavior.
MRI is also useful in identifying the patient’s stage of AD, telling doctors how far the disease has progressed. The more widespread the shrinkage of the brain, the more severe the stage of AD. Knowing the stage of AD can help doctors to customize treatment to the patient, instead of providing one-size-fits-all treatments. Furthermore, MRI helps distinguish AD from other neurodegenerative diseases and types of dementia [3].
Evolving Uses of Neuroimaging in Medicine
The use of neuroimaging tools to diagnose neurodegenerative diseases helps doctors to better treat patients, because these tools give the doctors more time to treat and slow the effects of neurodegeneration. Since chemical changes occur earlier in the disease progression, PET is the preferred method of diagnosis in the initial stages of any neurodegenerative disease. However, as the disease progresses, MRI becomes increasingly useful because it can detect shrinkage in the brain [3]. Both techniques together provide a more accurate diagnosis.
Unfortunately, most neurodegenerative diseases, including AD, are incurable. Moreover, AD patients suffer from a loss of identity over time, which leads to feelings of frustration and helplessness. Figure 3 shows how one artist with AD eventually forgot his own appearance—imagine forgetting how you look! An accurate diagnosis is important for helping doctors relieve such negative feelings in the patient, which is why we depend on neuroimaging. Neuroimaging data enable us to manage symptoms before they worsen and help families cope with the changes the patient experiences. New research is exploring the possibility of using MRI and PET to identify people who are at risk for developing AD so that they can be closely monitored, which can lead to even earlier diagnoses. Other research uses MRI and PET brain imaging to look for possible treatment options and ways to slow disease progression.
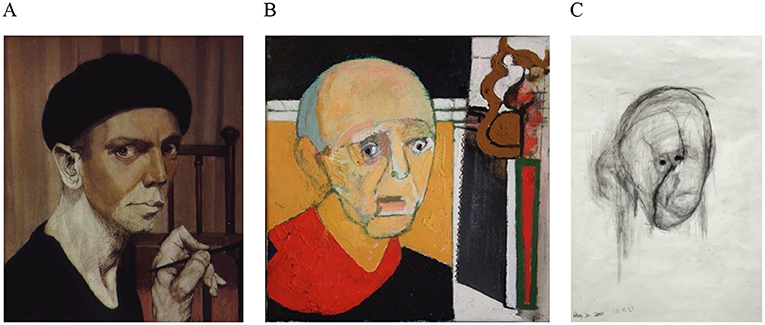
- Figure 3 - Progression of Alzheimer’s through the eyes of an actual patient.
- These self-portraits were painted by William Uterhmohlen, who was diagnosed with Alzheimer’s in 1995. He died in 2007. (A) This portrait was made in 1960 before his diagnosis. (B) This portrait was painted in 1997, soon after his diagnosis. (C) This portrait was painted in 2000. These self-portraits show how Uterhmohlen, like many other Alzheimer’s patients, began losing even memories of what he looked like (Image credit: Chris Boïcos Fine Arts, Paris; http://www.williamutermohlen.org/).
Overall, PET and MRI are great tools for diagnosing neurodegenerative diseases. Early detection can improve patients’ quality of life throughout the course of the disease and give patients time to prepare for the changes they will face. Researchers study PET and MRI images to gain a deeper understanding of neurodegeneration, to help develop new treatments, and to improve the existing treatments. One day, neuroimaging may even be the key to finding the cure for Alzheimer’s! However, it is important to note that neuroimaging is not a perfect solution, nor is it the only tool employed by doctors. It is one tool out of many that aids doctors and scientists in understanding, and ultimately curing, neurodegenerative diseases.
Glossary
Neuroimaging: ↑ Taking pictures of the brain through the skull to show the structure and/or function of the brain.
Neuro-degenerative Disease: ↑ A type of brain disease that causes wasting away of brain tissue over time. “Neuro” means nerve cell; “degenerative” means wasting away.
Alzheimer’s Disease: ↑ Type of neurodegenerative disease that is usually associated with long-term memory loss.
Dementia: ↑ A set of symptoms that occur when the brain is damaged by disease. Dementia is typically irreversible, worsens over time, and results in a loss of mental functions and reduced quality of life.
Hippocampus: ↑ A seahorse-shaped structure found on both sides of the brain. It is associated with learning, memory, and emotions.
Positron Emission Tomography: ↑ A neuroimaging technique that uses chemical tracers to track unusual brain activity.
Magnetic Resonance Imaging: ↑ A neuroimaging technique that uses magnetic fields and radio waves to take pictures of the brain.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Tan, S. Y., and Yip, A. 2014. Antonio Egas Moniz (1874-1955): lobotomy pioneer and nobel laureate. Singapore Med. J. 55:175–6. doi: 10.11622/smedj.2014048
[2] ↑ Loudjani, S., Narayanan, S., Haqqani, A., and Badhwar, A. 2020. How your blood knows your brain is sick. Front. Young Minds. 8:561561. doi: 10.3389/frym.2020.561561
[3] ↑ Johnson, K. A., Fox, N. C., Sperling, R. A., and Klunk, W. E. 2012. Brain imaging in Alzheimer disease. Cold Spring Harb. Perspect. Med. 2:a006213. doi: 10.1101/cshperspect.a006213
[4] ↑ Amanamba, U., Sojka, A., Harris, S., Bucknam, M., and Hegdé, J. 2020. A window into your brain: how fMRI helps us understand what is going on inside our heads. Front. Young Minds. 8:484603. doi: 10.3389/frym.2020.484603
[5] ↑ Berger, A. 2002. Magnetic resonance imaging. BMJ. 324:35. doi: 10.1136/bmj.324.7328.35