Abstract
The coronavirus pandemic has completely turned our reality upside-down, changing our perspectives and behavior in every aspect of our lives. We have had to modify family gatherings, school, work, and interactions with our friends and loved ones. New concepts such as Zoom meetings, social distancing, masks, PCR tests, quarantine, and shutdowns have become our norm. Early in the pandemic, we optimistically thought that once the vaccine became available, the pandemic would be controlled and the threat of COVID-19 would gradually subside. Within a year, a novel vaccine became available—but we are still not out of the woods. In this article, we discuss how novel COVID-19 mRNA vaccines have helped control the pandemic and some of the challenges we still face.
The emergence of COVID-19 in December 2019 has taken the world completely by surprise, swiftly spreading throughout the globe and infecting millions of men, women, and children. The scientific community along with the pharmaceutical industry were posed with the tremendous challenge of producing an effective vaccine that would hopefully stop the unprecedented spread of COVID-19. Remarkably, only a year into the COVID-19 pandemic, a vaccine was designed, manufactured, tested, approved, and used globally. Despite the billions of vaccine doses administered in massive, worldwide vaccination campaigns, we did not see the long-lasting protection against COVID-19 infection that we had hoped for. To be sure, the vaccine is extremely beneficial, preventing COVID-19-related hospitalizations, serious diseases, and deaths [1]. However, vaccinated individuals, even after repeated boosts, can still become infected and can transmit the disease to others. Before we address why this happens, we must first understand what vaccines are and how they work.
Vaccines—“Boot-Camp Training” for the Immune System
All vaccines contain an active ingredient, the vaccine immunogen, that stimulates the immune system to protect us. In the past, vaccines against viruses consisted of one of the three types of immunogens: inactivated, killed viruses; live, weakened viruses that cannot cause disease; or protein “pieces” of a virus, such as the spike proteins on the surfaces of some viruses that help them stick to and infect cells (Figure 1). When certain cells of our immune system, called B cells, encounter the viral immunogen in the vaccine, they respond by producing virus-specific antibodies that stick to and inactivate the virus (Figure 2). The B cells also produce a population of long-lived cells called memory B cells. Should we encounter the same virus in future, the memory B cells are quickly called into action, to flood the system with their virus-specific antibodies. Antibodies latch onto the invading viruses, preventing infection and protecting us against disease. Thus, the immune system “trains” on the harmless viral immunogens in the vaccine, learns how to beat and prevent infection. Then, should we encounter the actual virus in the future, the immune system can be called upon to prevent disease.
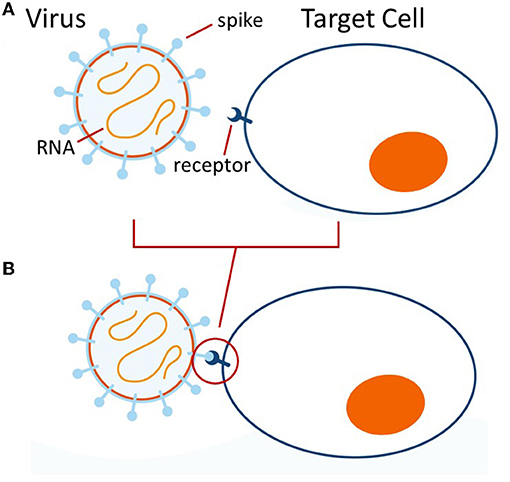
- Figure 1 - (A) SARS-CoV-2 virus contains an RNA genome and is decorated with spike proteins.
- (B) The spike proteins can bind to a molecule on the target cell (the cell to be infected) called a receptor, which sticks the virus to the target cell and leads to infection. (Figure adapted from https://www.youtube.com/watch?v=wchaaU0wMcQ).
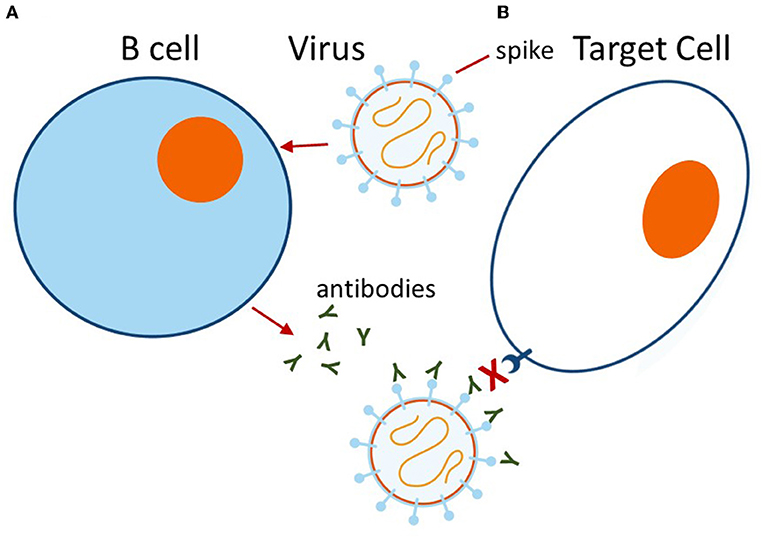
- Figure 2 - (A) When a virus encounters a B cell, the B cell responds by producing antibodies (the small Y-shaped structures) specific for the viral spike protein.
- (B) These antibodies bind to the viral spike proteins, blocking them from sticking to the receptor on the target cell and thus preventing infection. (Figure adapted from https://www.youtube.com/watch?v=wchaaU0wMcQ).
Vaccines are amazingly effective. Most of us have received childhood vaccines that give us life-long immunity. For example, at 12 months old, we get the triple MMR vaccine, which protects us against measles, mumps, and rubella for years! Many of us expected that the COVID-19 vaccine would be equally effective: that it would provide long-lasting immunity against the SARS-CoV-2 coronavirus and that life would quickly return to normal. This has not been the case.
The COVID-19 vaccine is revolutionary. It does not contain one of the typical immunogens but instead contains messenger RNA (mRNA)—the “instructions” for producing the viral spike protein. Some people argue that this new mRNA technology might explain the limited protection against infection with SARS-CoV-2. Is it true?
The Coronavirus Vaccine Revolution
If we think of traditional vaccines as containing viral “hardware”—that is, the actual viral proteins—then mRNA vaccines against SARS-CoV-2 can be considered to contain viral “software” that carries the message telling cells how to make the spike protein [2]. The idea is that, when spike-encoding mRNA is injected into the muscle, it is then picked up by special cells of the immune system that produce “fresh” spike protein, which can then stimulate the production of antibodies by B cells.
Two questions have arisen regarding mRNA vaccines. First, is mRNA dangerous? Second, are mRNA vaccines less effective than traditional “hardware”-containing vaccines? In terms of the first question, some people have argued that the injection of mRNA could be dangerous, causing harmful side effects even years later. Childhood vaccination has been around for decades and has saved the lives of billions of kids around the world—without any long-term negative effects. Seven of the vaccines that are given to kids as part of the routine vaccination schedule (which consists of 14 vaccines, in most countries), actually contain live, weakened RNA-containing viruses: polio, flu, hepatitis A, rotavirus, mumps, measles, and rubella. These vaccines deliver RNA from all of the virus’s genes because these weakened viruses reproduce throughout our bodies for weeks—with no ill effects or long-term negative consequences. From this information, it is very likely that the injection of tiny amounts of viral mRNA vaccines into the muscle is not dangerous.
In terms of the second question, we generally expect a successful vaccine to effectively protect us against infection for years. The COVID-19 mRNA vaccines do cause the production of antibodies that inactivate SARS-CoV-2 and protect us from serious life-threatening diseases [1]. However, the antibodies decrease within just months after vaccination, and it is extremely common for vaccinated individuals to become infected. In fact, vaccinated people can be infected, recover, and then get infected again! Is this because the vaccine is not strong enough? Probably not. Hundreds of millions of people worldwide have been infected with SARS-CoV-2 and over 98% have recovered. However, an actual bout with COVID-19 does not promise long-lasting protection against SARS-CoV-2. Despite being naturally infected, millions of people who have recovered have multiple, recurrent infections. This tells us that having multiple infections with SARS-CoV-2 is not due to the vaccine not working well enough—it is apparently a basic feature of coronaviruses themselves.
Lessons From Animal Coronaviruses
In the 1930s, a coronavirus called infectious bronchitis virus was shown to infect chickens. Many more coronaviruses have been discovered that infect cats, dogs, cows, and pigs [3]. Usually, animals get infected, recover, and get infected again! In fact, numerous veterinary vaccines have been produced to protect livestock and pets against coronaviruses, and they all seem to perform the same way—they protect animals against serious, life-threatening diseases but not against repeated infections [3]. Does this sound familiar? Maybe the writing has been on the wall!
In contrast to viruses such as measles, polio, and smallpox—for which effective, long-lasting vaccines exist—coronaviruses simply do not fit our expectations of how vaccines should perform. There are many families of viruses, each with its own biological characteristics. Some viruses seem to activate the immune system in a way that protects us from reinfection for the long term (whether through natural infection or vaccination)—but others do not. For example, smallpox has actually been eradicated through global vaccination campaigns but, in complete contrast, there are some viruses, for which vaccination is a total failure—there are no effective vaccines against HIV, the cause of AIDS.
The COVID-19 Vaccine Verdict
We must remember that SARS-CoV-2 is a member of a unique virus family—the coronaviruses. As already observed, coronaviruses do not seem to generate durable and efficient immunity when they infect people or animals. Pets, livestock, and people that suffer from coronavirus infections and recover do not develop long-lasting immunity against reinfection. Vaccination of animals (and people) against coronavirus diseases provides temporary protection against serious life-threatening diseases but does not provide effective, life-long protection against reinfection. This seems to be the pattern for this whole family of viruses. So yes, the writing has been on the wall—maybe we should have predicted that vaccines against COVID-19 would not keep us immune for life.
This knowledge about coronaviruses should better prepare us against future emerging coronaviruses that could infect humans. While the COVID-19 pandemic has led to amazing technological advances including the development of revolutionary mRNA “software” vaccines, we must accept that the biology of the coronavirus family poses even more challenges that still need to be met. How do we outsmart coronaviruses so that we are better prepared for future pandemics? Maybe your generation of scientists will help to answer this important question!
Acknowledgments
The authors would like to thank their former teachers who profoundly influenced their lives and careers: Ofra Graph, Ron Kessler, Itsik Ohad, and George Palade.
Glossary
Pandemic: ↑ A disease that rapidly spreads worldwide, infecting a large number of people.
Immunogen: ↑ A molecule that causes an immune response in the body. Foreign proteins from bacteria and viruses are common immunogens.
Spike Protein: ↑ The protein on the surface of the SARS-CoV-2 virus that specifically sticks to a receptor molecule on the target cell and results in infection.
B Cells: ↑ Cells of the immune system that respond to immunogens by producing molecules called antibodies, which can stick to immunogens and inactivate them.
Antibodies: ↑ Proteins produced by B cells that can bind viruses and thus prevent their sticking to a receptor molecule on the target cell.
SARS-CoV-2: ↑ Severe acute respiratory syndrome coronavirus 2—the virus that causes COVID-19.
Messenger RNA (mRNA): ↑ Molecules that carry the genetic information that instructs the production of proteins.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Haas, E. J., McLaughlin, J. M., Khan, F., Angulo, F. J., Anis, E., Lipsitch, M., et al. 2022. Infections, hospitalisations, and deaths averted via a nationwide vaccination campaign using the Pfizer-BioNTech BNT162b2 mRNA COVID-19 vaccine in Israel: a retrospective surveillance study. Lancet Infect. Dis. 22:357–66. doi: 10.1016/S1473-3099(21)00566-1
[2] ↑ Weissman, D. 2022. Messenger RNA therapies finally arrived. Sci. Am. 326:54.
[3] ↑ Sariol, A., and Perlman, S. 2020. Lessons for COVID-19 immunity from other coronavirus infections. Immunity. 53:248–63. doi: 10.1016/j.immuni.2020.07.005
