Abstract
Blood is the liquid that looks red when you cut or scrape your skin. People think blood is bad because they see it when they hurt themselves, when people are sick at hospital, and in scary movies. But blood is needed to keep our bodies alive and well. So, what happens when you bleed? And what happens if blood flow is blocked? In this short article, we will explain how and why blood is good. We will also tell you how doctors and scientists can help with problems of the blood.
Key Points
Healthy blood and scabs are good for our wellbeing. Too much bleeding and blood clots are unhealthy. Doctors and scientists are working together to stop bleeding and blood clots and to help people recover from blood illnesses.
Blood
Blood moves through the body inside bendy tubes called blood vessels. The movement of blood is called blood flow. Blood flows through blood vessels like water flows through a hose pipe. One reason the blood flows through the blood vessels is to take food and oxygen to various parts of the body. Oxygen travels in the blood on mini life rafts called red blood cells. These cells contain a red protein called hemoglobin. The blood flow allows the body’s muscles and organs to do their jobs. For example, blood flowing to your brain allows you to think, blood flowing to your legs allows you to walk, and blood flowing to your mouth allows you to talk and eat. It is important to keep blood flowing through the blood vessels because blood keeps the body working normally. To keep the blood inside, the blood vessels are lined with tiny flat cells called endothelial cells, which act as barriers to stop the blood from leaking out. But sometimes things go wrong! Examples of problems with the blood include cuts and blood clots.
Cuts and Scabs
When you fall over and scrape your skin, the tiny blood vessels under your skin break. Then, blood flows out of the blood vessels and onto your skin. This is called bleeding. Nose bleeds often happen when a person bangs their nose on something, causing the blood vessels in the nose to break. Nose bleeds can also happen on their own, because of changes in air pressure or because the vessels inside the nose can be a bit leaky. To stop the bleeding, the blood and blood vessel launch a fast response [1]. First, sticky little cells in the blood called platelets join together at the cut site, in a process called blood clotting. Clotting plugs the holes in the broken blood vessels and stops the bleeding.
Also, helper cells called white blood cells arrive to protect the body against germs and dirt. These cells help fix the blood vessel, too. New endothelial cells form where the blood vessel was broken, to mend the blood vessel and return blood flow to normal. Because the cells are so small, we can only see them when they have joined together in a clump on the skin. This team of cells and the stringy ties that connect them is called a scab. Scabs change color, size, and shape over several days as cells are working to fix the broken blood vessels. When the scabs have finished their job, they fall off! You can think about cuts and scabs this way: imagine pulling the plug out from a bathtub or sink. The water flows down the drain. You can slow the flow by using your hand to cover the drain, and you can completely stop the flow by replacing the plug.
If the skin is bleeding a lot, there are a few actions that can help (Figure 1). First, it is helpful to press on the injury, to squeeze the flowing blood away from the broken blood vessels. It can also be helpful to raise the injured body part high into the air because this makes it harder for blood to reach the broken vessel. To protect broken blood vessels and speed up the repair process, a bandage or band-aid can be wrapped around the injured area. It is important to watch the skin for a few days after the healing has finished, to check that everything looks normal. If a person has a large cut or needs a surgery, doctors can use small pieces of string, called stitches, to tie the injured skin back together. During surgery, doctors can also use special instruments to reduce the amount of bleeding.
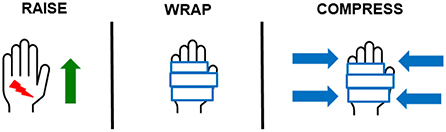
- Figure 1 - Three tips to help stop bleeding.
Scientists are trying to find out about the cells that take part in blood vessel repair [1, 2]. For example, they want to know how the cells get to the right place on time, how they communicate with other cells around them, and what they do to help with the vessel repair.
Blood Clots
A blood clot (also called a thrombus) is a squishy lump of blood cells. It is good when clots form to stop the blood from flowing out of the body, but it is bad if clots stop blood flowing inside a blood vessel—which happens in a small number of people (Figure 2). Blood clots are made up of platelets, white blood cells, and red blood cells. Blood clots happen inside a blood vessel when the blood is thicker than usual, when the inner blood vessel wall is injured, or when the blood flow is reduced [3]. Young people do not usually get blood clots inside their blood vessels. Blood clots inside blood vessels can stop the blood from getting to important body parts, like the lungs, heart, and brain.
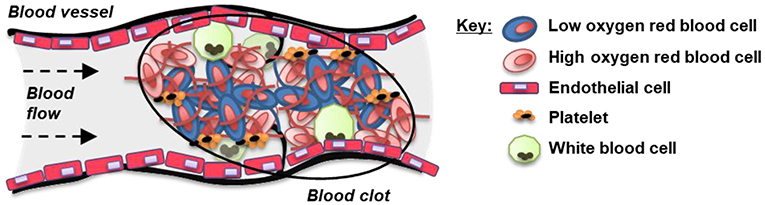
- Figure 2 - Sometimes blood can clot inside a blood vessel.
- Blood clots contain various types of cells and some sticky proteins that hold the clot together. If the clot is too big, it can block the blood flow, and this can stop the blood from getting to important body parts like the heart, brain, or lungs.
Thankfully, there is a bodily response that can help to break up the clot [4]. White blood cells and endothelial cells work together to reduce the size of the clot and to make new channels within the clot, which allows blood to flow through and around the clot. This process is called thrombus resolution, but unfortunately, it can take a long time. Some people have other problems after a blood clot, including leg pain, swelling, and difficulty walking. You can think about this process like this: imagine some cars traveling down a road. If there is an accident, all the cars must slow down or stop. Next, emergency service vehicles arrive to help with the accident and clear the road, so that cars can travel normally again.
Doctors can give people with blood clots medicine to stop the blood from clotting. These medicines work by making the blood less thick and slowing down the process of blood clotting. The medicines include drugs called anti-coagulants. Doctors can also provide tights or stockings that press on the outside of the arm or leg, to keep the blood flowing. Another thing that doctors can do is to break up the blood clot by giving the person some medicine or by using special hospital equipment.
Scientists are trying to find out how and why the blood cells clot together and how the clot is broken down [5]. A big goal for scientists is to find ways to stop clots from forming inside blood vessels and to speed up thrombus resolution.
Glossary
Red Blood Cells: ↑ Life-raft cells that carry air to various parts of the body.
Hemoglobin: ↑ The red protein responsible for transporting oxygen in red blood cells.
Endothelial Cells: ↑ Flat cells that form a barrier along the inside of blood vessels.
Platelets: ↑ Small, sticky cells that join together to plug broken blood vessels.
White Blood Cells: ↑ Helper cells that protect the body against infection.
Blood Clot: ↑ Also called a thrombus; a collection of blood cells that clump together to heal a wound (good) or inside a blood vessel (bad).
Thrombus: ↑ A blood clot inside a blood vessel.
Thrombus Resolution: ↑ The bodily process that removes the thrombus.
Anti-Coagulant: ↑ A type of drug that thins the blood to reduce blood clotting.
Conflict of Interest
Author AS was employed by Mercyhealth.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Singer, A. J., and Clark, R. A. 1999. Cutaneous wound healing. N. Engl. J. Med. 341:738–46. doi: 10.1056/NEJM199909023411006
[2] ↑ Evans, C. E., Iruela-Arispe, M. L., and Zhao, Y. Y. 2021. Mechanisms of endothelial regeneration and vascular repair and their application to regenerative medicine. Am. J. Pathol. 191:52–65. doi: 10.1016/j.ajpath.2020.10.001
[3] ↑ Bagot, C. N., and Arya, R. 2008. Virchow and his triad: a question of attribution. Br. J. Haematol. 143:180–90. doi: 10.1111/j.1365-2141.2008.07323.x
[4] ↑ Modarai, B., Burnand, K. G., Humphries, J., Waltham, M., and Smith, A. 2005. The role of neovascularisation in the resolution of venous thrombus. Thromb. Haemost. 93:801–9. doi: 10.1160/TH04-09-0596
[5] ↑ Furie, B., and Furie, B. C. 2008. Mechanisms of thrombus formation. N. Engl. J. Med. 359:938–49. doi: 10.1056/NEJMra0801082