Abstract
In the past, plants were the only medical resources available to people. Although plants were used a lot, sometimes they had dangerous effects. The evolution of science has allowed us to separate the helpful and dangerous compounds from various plants. An example is Cannabis sativa, also known as marijuana or weed, one of the most commonly used recreational drugs worldwide. These plants produce hundreds of compounds, called cannabinoids. The two most famous cannabinoids are tetrahydrocannabinol (THC), which produces the “high” sensation and might cause some of the negative effects of cannabis, and cannabidiol (CBD), which might be useful for treating certain diseases. In this article, we will explain how CBD can be used to treat epilepsy, a disease that affects people’s brain function. But remember: we are talking about the use of cannabinoids for therapeutic purposes only, not recreational use of marijuana.
Epilepsy: A Disorder of the Nervous System
The human body is an amazing machine, and the nervous system is an important part of it. The nervous system, which contains the brain, spinal cord, and nerves, controls functions that are both under our control, such as thinking and moving, and those that are controlled without thinking about them, like heartbeat and bowel movements.
Imagine that your brain is a school, made up of a team of teachers and students: the neurons. Neurons are an important cell type within the nervous system, and they pass and receive information all the time, controlling many body functions. Teachers and students must talk to each other to exchange information. This process takes place in classrooms. These are the synapses: areas where two neurons meet to communicate. The words spoken are neurotransmitters, chemical signals responsible for conversations between neurons. But sometimes everyone tries to communicate at the same time, and the activities in the school go wrong. This happens in the brains of people with epilepsy, the most common disease of the nervous system [1].
Epilepsy is a disease in which people’s brains sometimes emit incorrect signals, due to the irregular activity of neurons. These signals trigger epileptic seizures, which are characterized by simultaneous and excessive neuron activity in the brain (Figure 1) [1]. Epilepsy may have several causes, including lack of oxygen in the brain during childbirth, problems with metabolism or the immune system, high fever, a strong blow to the head, infections, and even the presence of certain genes. Intense emotions, specific noises, odors, lights, alcohol intake, or sleep deprivation can trigger seizures in people who suffer from epilepsy [1].
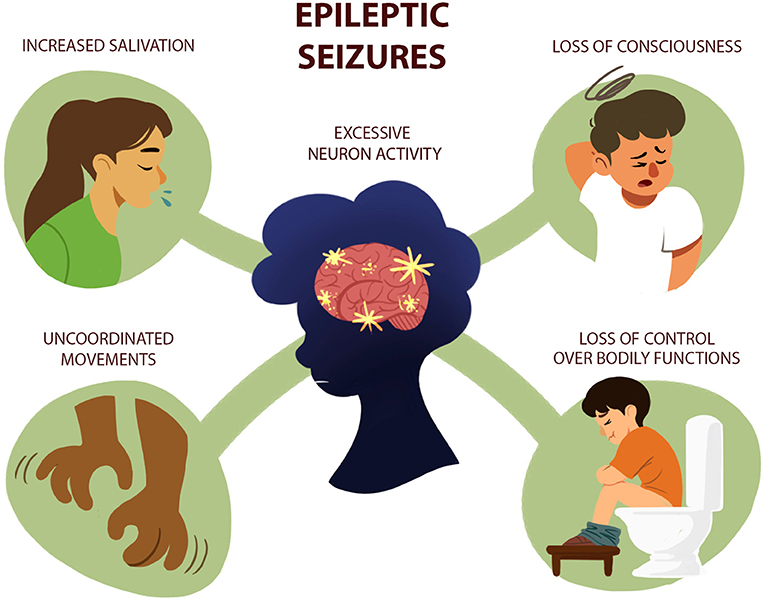
- Figure 1 - Epileptic seizures are caused by excessive and simultaneous neuron activity in the brain—like everyone talking at once in a classroom.
- Symptoms of epileptic seizures can include increased salivation, uncoordinated movements, loss of control over bodily functions (like peeing or pooping) and temporary loss of consciousness.
The incorrect neuron signaling in epilepsy may occur in one or many regions of the brain. For example, it can affect the frontal lobe (behind the forehead), triggering uncoordinated movements. It can affect the temporal lobes (the left and right sides of the brain), which process emotions and are important for short-term memory. In the parietal lobe (top of the head), incorrect signaling can cause sensory changes. And, in the occipital lobe (back of the head), improper signaling can generate visual changes. In most cases, seizures also result in a temporary loss of consciousness.
Epilepsy is a treatable disease, but 30% of epilepsy patients do not respond well to common treatments [2]. Therefore, new treatment options are needed. Without effective treatment, epileptic people have reduced chances of living normal lives. Luckily, there are scientific studies seeking new treatment options!
Effects of Marijuana Compounds
One of those studies uses substances from Cannabis sativa, a plant also known as marijuana, pot, or weed. You may be wondering how a plant used as a recreational drug could also be used to treat diseases! For centuries, plants were the only medicines available to people, and marijuana has been used for a long time to treat diseases, due to its effects on the brain. When marijuana is overused, however, a person might hear or see things that do not exist and might experience memory loss and other potentially dangerous side effects [3]. Scientists discovered that marijuana’s many effects are due to multiple chemical components, called cannabinoids, that are contained by the plant. Among them, tetrahydrocannabinol (THC) and cannabidiol (CBD) are the most important ones [3].
THC is the cannabinoid that can alter a person’s perception of the world, by changing brain function. People enjoy its effects, but overuse eventually results in difficulty with thinking, memory loss, mood swings, and negative effects. For this reason, marijuana is often considered a drug of abuse. In contrast, CBD does not cause negative effects in the brain. This cannabinoid has the most medicinal applications. It protects the brain, decreases depressive thoughts, and eases symptoms of other brain diseases, such as epilepsy [4]. But how does CBD work in the brain?
Discovery of a New Chemical System in the Brain
By studying cannabinoids, scientists discovered a new chemical system in the brain, named the endocannabinoid system. The endocannabinoid system has three main parts. First, we have the endocannabinoids (eCBs), which are substances similar to cannabinoids but produced by the body. eCBs belong to the family of neurotransmitters, which pass information between neurons. eCBs bind to the second component of the eCB system, cannabinoid receptors. eCBs and their receptors work like a key and a lock—when the key is inserted into the lock, the “door opens” and a signal is transmitted from the outside of the cell to the inside. There are two types of cannabinoid receptors, called CB1 and CB2. Certain enzymes are the third part of the system. Enzymes control the process—they produce and remove eCBs, ensuring that they are only present when needed.
Did you know that neurons produce many kinds of neurotransmitters? Tiny “bags” within the nerve cells, called synaptic vesicles, produce and store most neurotransmitters. Neurons communicate with each other by releasing these “bags.” Do you remember the comparison of neurons to teachers and students? Although they can all learn from each other, the teacher usually transmits more information to the student. In the brain, the “teacher” neurons (called presynaptic neurons) release neurotransmitters into the spaces between the two neurons, called the synaptic cleft. The information reaches “student” neurons (called postsynaptic neurons) and binds to the receptors on their surfaces (Figure 2). This signal transmits information from one cell to the other.
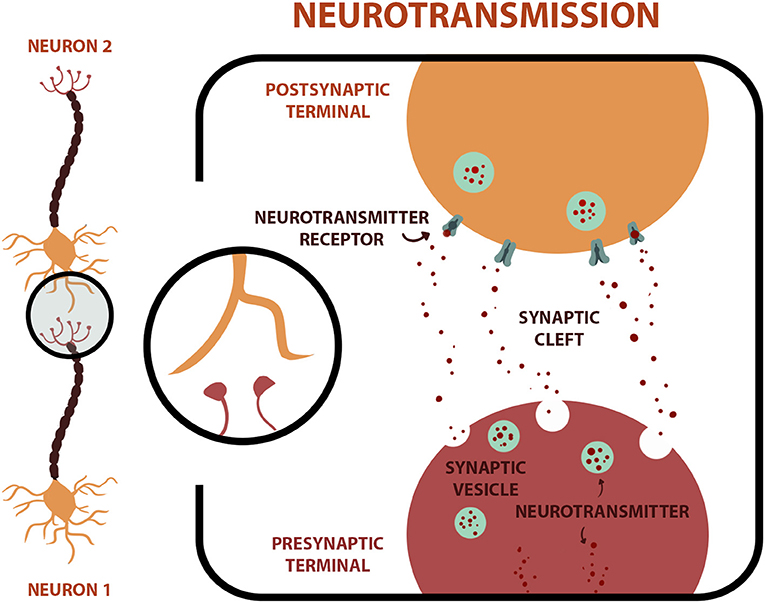
- Figure 2 - Neurons communicate with each other across a space called the synaptic cleft in which neuron 1 (pre-synaptic) communicates with neuron 2 (postsynaptic).
- In the close-up right image, synaptic vesicles inside the “teacher” (presynaptic) neuron release neurotransmitters into the synaptic cleft. These molecules bind to receptors on the “student” (postsynaptic) neuron.
The endocannabinoid system is somewhat different! eCBs are produced only when we need them. They are not stored in synaptic vesicles and are released in the opposite direction, which is known as retrograde neurotransmission. This is like students transmitting information to teachers (Figure 3) [5]. Both eCBs and cannabinoids from marijuana act through the brain’s CB1 and CB2 receptors.
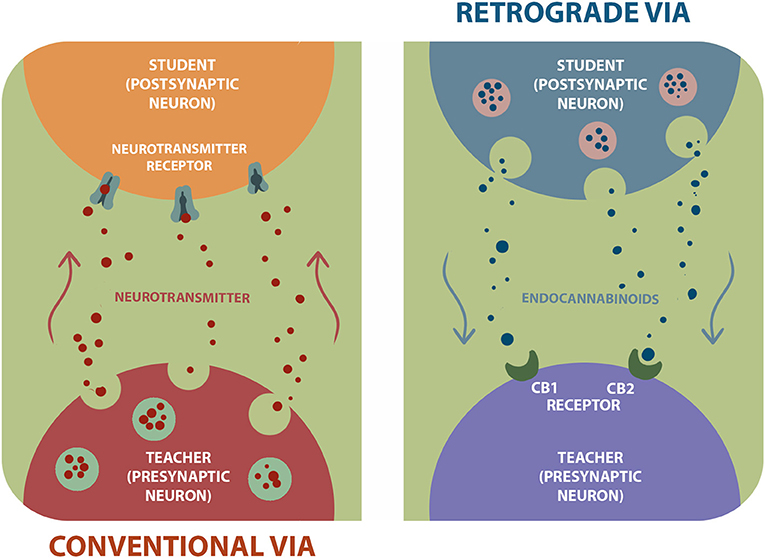
- Figure 3 - On the left image, we show the conventional via in which “teacher” neuron (presynaptic) releases neurotransmitters.
- These neurotransmitters bind to “student” neuron (postsynaptic) receptors. On the right side, the image represents the retrograde via, in which neurotransmission happens backwards: endocannabinoids released from “student” neuron (postsynaptic) bind to receptors CB1 and CB2 on “teacher” neuron (presynaptic).
Cannabinoid receptors are found throughout the body. CB1 is mostly found in the brain, where this receptor plays a role in attention, memory, emotions, learning, pleasure, appetite, mood, pain, and motor ability. CB2 receptors help to control the immune system, which protects the body from disease-causing organisms [5]. Since there are cannabinoid receptors throughout the body, the endocannabinoid system participates in the development and proper functioning of many structures, including the brain. But in some diseases, like epilepsy, the endocannabinoid system does not work well [4]. Therefore, substances that regulate the function of the endocannabinoid system might be a promising way to treat diseases like epilepsy.
Use of CBD for Epilepsy Treatment
Scientific studies suggest that CBD reduces seizures in different types of epilepsy that affect adults and children. In addition, CBD has fewer adverse effects when compared to other medications used to treat epilepsy. Although the results are promising, larger clinical studies are needed.
Scientists still do not fully understand how CBD works in the brain to help control epilepsy. One thing we know is that THC binds to cannabinoid receptors in the brain, which mediates its effects in that organ, but CBD does not bind to those receptors. Instead, CBD seems to act on other receptors and pathways in the brain to facilitate the functioning of the endocannabinoid system. CBD can stimulate the production and release of eCBs, which seems to inhibit the excessive activity of neurons that causes epileptic seizures [4]. Although CBD appears to be safe and has promising results in the treatment of epilepsy, further studies are needed to determine exactly how it works [1, 2]. Science is done that way—each research study is a piece of the puzzle and, the more pieces we have, the greater the chances that we can help people.
Conclusion
The study of cannabis and the endocannabinoid system can provide important scientific discoveries. Separating CBD from other marijuana compounds and using it to treat epilepsy can be a great alternative for patients that suffer from this disease. When we talk about the efficacy and safety of CBD as a medicine, we are not saying that smoking marijuana is safe—it contains several compounds that might be bad for your health, including THC. Even CBD is not a miraculous compound! Like any other medicine, it may work well for some people but not for others. That is why only doctors can advise us about which medicines to take. This article is just one example of how science can make discoveries that can have positive impacts on our lives, including treatments for important diseases!
Glossary
Neurotransmitters: ↑ Signaling molecules produced by neurons. Through them it is possible to send information to other cells.
Epilepsy: ↑ A neurological disorder that affects the activity of neurons in the brain and causes seizures.
Cannabinoids: ↑ Natural or artificial compounds present in marijuana. Cannabinoids bind to the cannabinoid receptors CB1 and CB2.
Endocannabinoids: ↑ Neurotransmitters produced by our body, similar to cannabinoids, that helps regulate various body processes.
Receptors: ↑ Cellular structures that allow the interaction between the cell and specific molecules. This lock-and-key interaction can lead to the transmission of signals inside and outside the cells.
Synaptic Vesicle: ↑ Compartments that store various neurotransmitters that are released at the synapse.
Synaptic Cleft: ↑ Small space between pre and post neurons where neurotransmitters are released to perform their function, binding to receptors and generating a physiological response.
Retrograde Neurotransmission: ↑ Process by which a neurotransmitter, such as endocannabinoids, is released by postsynaptic neurons and “travels backwards” to bind to receptors on the presynaptic neurons.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This work was supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico - (CNPq) (474528/2012-0, 483184/2011-0, and 477867/2010-3), Fundação de Amparo à Pesquisa do Estado de Minas Gerais - (FAPEMIG) (APQ-01756-10, APQ-02198-14, APQ-03950-17, and APQ-01899-18), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001, and Instituto Nacional de Ciência e Tecnologia em Dengue e Interação Microrganismo Hospedeiro (INCT em Dengue).
References
[1] ↑ Falco-Walter, J. J., Scheffer, I. E., and Fisher, R. S. 2018. The new definition and classification of seizures and epilepsy. Epilepsy Res. 139:73–9. doi: 10.1016/j.eplepsyres.2017.11.015
[2] ↑ O’Connell, B. K., Gloss, D., and Devinsky, O. 2017. Cannabinoids in treatment-resistant epilepsy: a review. Epilepsy Behav. 70(Pt B):341–8. doi: 10.1016/j.yebeh.2016.11.012
[3] ↑ Mechoulam, R., Hanuš, L. O., Pertwee, R., and Howlett, A. C. 2014. Early phytocannabinoid chemistry to endocannabinoids and beyond. Nat. Rev. Neurosci. 15:757–64. doi: 10.1038/nrn3811
[4] ↑ Zuardi A. W. 2008. Cannabidiol: from an inactive cannabinoid to a drug with wide spectrum of action. Revista Brasileira de Psiquiatria 30:271–80. doi: 10.1590/s1516-44462008000300015
[5] ↑ Lopes, J. B., Bastos, J. R., Costa, R. B., Aguiar, D. C., and Moreira, F. A. 2020. The roles of cannabinoid CB1 and CB2 receptors in cocaine-induced behavioral sensitization and conditioned place preference in mice. Psychopharmacology. 237:385–94. doi: 10.1007/s00213-019-05370-5
