Abstract
The heart is the organ in charge of pumping blood to the rest of the body. But the heart can get sick, and we want to know how to best mend it. Sometimes, doctors can give medicines or do heart surgery to treat heart problems. But some medicines may not work for everyone, and surgeries can be very difficult. Now we have special computer games to better guide these decisions: cardiac simulations. Cardiac simulations are like having a twin of the heart in the computer. Doctors can try different medicines in the simulation without putting the patient at risk. They can also use the heart simulation to practice for surgery. They can train using the simulation until they are ready, and then do the surgery in the real world. With the help of computer simulations, we can find the best way to help sick hearts.
What Is That Sound Inside The Chest?
If you put your head close to someone’s chest, you can hear a sound like “dum-dum,” which is the heart beating and pumping blood.1 Your heart is about the size of your fist, and its task is to send blood throughout the body, so every body part has enough oxygen and nutrients to work properly. Like the rest of the body, the heart can be healthy and strong or sick and weak. Most of the heart is made of muscle, and every time the heart beats it is doing exercise. If the heart needs to beat faster, like when you are playing sports, it will grow stronger. However, if the heart does not work out enough, it can get weaker.
What causes the heart to make that sound when it beats? In addition to muscle, the heart also has valves. Imagine that you live in a submarine and your bedroom has a window. If you open the window, water will come into the room until you close the window. Then, if you open the door, the water that came in will flow out to the rest of the submarine. In the heart, the bedroom is called a ventricle, and the window and door are the valves that let the blood move into and out of the heart (Figure 1). But there is no need for anyone to be inside the ventricle to open the valves: when the blood pushes enough, the valves open and blood flows through. This push, when the blood bumps against the valves, is the “dum” we hear. Unfortunately, very much like doors or windows, sometimes the valves might not close or open completely and that can be a problem.
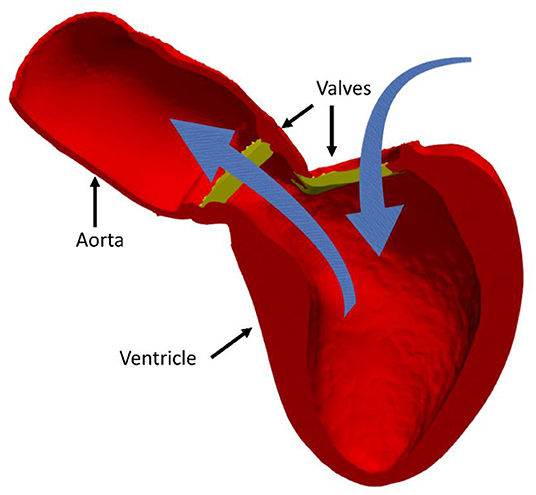
- Figure 1 - The left ventricle (red) with its valves (yellow).
- The arrows indicate the direction of the blood flow. Once the blood leaves the left ventricle, it goes out to the rest of the body through the largest artery in the body, called the aorta.
Taking Photos of The Heart
When there is a problem in the heart and the doctors do not know exactly what is going on, they cannot simply take the heart out to have a look. But they can use special photographs to see what is happening inside the heart. You have probably heard of x-rays, which are special photographs that allow doctors to look inside your body to see how your bones are. Similarly, we can use other types of “rays” to see the heart. These scans include magnetic resonance imaging (MRI), which uses magnets; computerized axial tomography (CAT), which uses lots of x-rays; and echocardiography, which uses sounds to create images of the heart. Echocardiography is the safest technique, and MRI is very safe too, if patients do not have any metal implants inside their bodies. CAT scans use radiation, so having multiple CAT scans can increase the risk of developing certain cancers. You can read more about how MRI, CAT and echocardiography work in the linked Frontiers for Young Minds articles! [1–3].
Although these techniques are used very often by doctors, the heart photos can be tricky to understand. The heart has height, depth, and width, but the pictures only show a slice. Think of studying a loaf of bread but not seeing the whole loaf, only one slice at a time. We call these slices 2D images. If we stack all the 2D images together, we get a 3D image. It is much easier for doctors to understand 3D images of the heart than 2D images. Thus, 3D images can save time and money and improve the ability of doctors to know what is going on with the heart.
So, how do we make a 3D heart image? Most 2D images show not only the heart, but also the lungs and other organs heart doctors are not interested in. On top of that, the images are usually in black-and-white. The first step is to tell the computer what parts of the photos show the heart. This technique, called segmentation, is just a fancy way of coloring. Like in a coloring book, the tricky part is not coloring outside the lines. When all the 2D images are segmented, the computer can discard everything that is not the heart and then assemble all the 2D images together. Now the heart looks much like a model that you can move around or look inside, rather than just a set of photos (Figure 2).
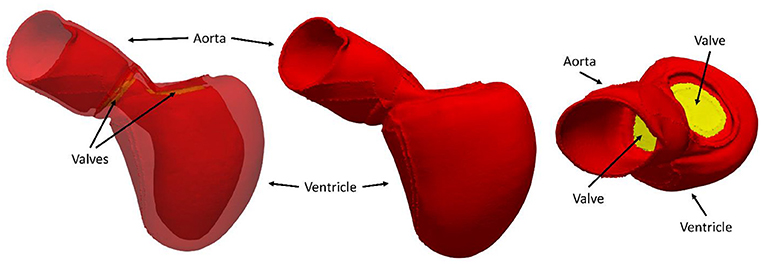
- Figure 2 - 3D model of the left ventricle and aorta.
- The image in the center corresponds to the 2D image in Figure 1. We can make this image more transparent so that we can see inside it (left), or we can rotate it to see how it looks from various angles (right).
Your Heart: The Videogame
If you are playing basketball, we could figure out when the ball is going to go through the hoop by using physics, if we know things like the direction of the ball and how hard you shoot it. Similarly, we can predict how the heart is going to move when it is healthy and when it is sick. Cardiac simulations are like computer games, in which we use ideas from physics to understand how the heart will work. Like car-driving simulators, the more realistic, the better.
Before every heartbeat, there is an electric wave that flows over the heart muscle, and this signal makes the muscle squeeze. Some drugs affect how the electric wave moves and how fast, so understanding the physics of the electric wave helps us understand how well some drugs will work on patients. As in some videogames, the heart simulation allows us to try multiple times—we do not run out of lives!
To pump blood out of the heart, the whole heart needs to squeeze at the same time. In some people this does not happen, and one side of the heart squeezes before the other. These people can have a device placed in the heart that makes sure both sides squeeze at the same time. One question that doctors have is where to place the device. Since we cannot try all the possible locations in the patient directly, we can create a digital copy of the heart and do simulations to test all possible locations for the device, to find the best one [4].
In other cases, the heart valves are not working properly and need to be replaced. This surgery is not easy, and it can be useful for the doctors to know the best location to repair. One solution is to use simulations, try all the possible places, and choose the best one. Once again, everything is done on the computer, so no harm has been done to the patient!
In addition to helping doctors learn more about why a heart is sick, cardiac simulations can also help us understand more about the healthy heart.2 With heart images from multiple people, we can create a digital population of hearts and look at their differences and similarities. For example, using simulations, we found out that small differences in the shape of the heart can have a big impact on how it works [5].
Better Consoles, Better Games, Better Future
This heart videogame is still in its early stages of development. The more we learn about the heart, the more complex we see it is, so our simulations need to become more realistic. We need new and more powerful consoles. The computers we use are more powerful than 90,000 PS5s put together. These supercomputers help us do faster research and test our cardiac simulations more accurately. Supercomputers are not only bigger but also smarter than most computers. Instead of doing one thing at a time, they can do several things at once. Computer scientists help to make the simulations faster, so that we can see the results as soon as possible.
Although there are still many things we do not know about the heart, now we can do research using the computer to try to learn more every day. Cardiac simulations are already available and can help doctors to mend broken hearts without risking the lives of patients. There is much work yet to do, so this area of study needs doctors, engineers, computer scientists, and mathematicians. Many researchers around the globe will continue to work together, using supercomputers and cardiac simulations, to build a better future.3
Funding
CR has received funding from the European Union’s Horizon 2020 Research and innovation programme under the Marie Sklodowska-Curie Grant Agreement No. 764738. PL holds a Wellcome Trust Senior Research Fellowship (209450/Z/17/Z) and is supported by BHF [PG/16/75/32383]. SN is supported by NIH R01-HL152256, ERC PREDICT-HF 453 (864055), BHF (RG/20/4/34803), and EPSRC (EP/P01268X/1). This work was supported by the Wellcome/EPSRC Centre for Medical Engineering [WT 203148/Z/16/Z] and by the BHF Centre for Excellence (RE/18/2/34213).
Glossary
Valve: ↑ Part of the heart in charge of letting blood in or out between different parts of the heart. They can open and close depending on the blood pressure.
Ventricle: ↑ Part of the heart where the blood is stored right before being pumped to the rest of the body. Is the region where the heart muscle is stronger.
Magnetic Resonance Imaging (MRI): ↑ Technique to take photos of the inside of the body by using powerful magnets and the properties of the water in the body.
Computerized Axial Tomography (CAT): ↑ Technique to take photos of the inside of the body by using x-rays and a “contrast agent,” a liquid that lights up when the x-rays hit it.
Echocardiography (or Echo): ↑ Technique to take photos of the inside of the body by using sounds and checking where the sound waves bounce back, similarly as how bats can “see” in the dark.
Segmentation: ↑ Technique to select specific parts of 2D images by coloring them and discard the rest. In our case, we select the heart out from the rest of the body.
Simulation: ↑ Simplified replication of an event to help studying it. Computer simulations use computers to help, and cardiac simulations study the heart.
Supercomputer: ↑ Very powerful computers used in science to speed up the process of solving problems.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
1. ↑You can experience this by downloading the echoes app and recording your heart sounds: Echoes app: https://www.echoesapp.org/
2. ↑https://vimeo.com/574341737
3. ↑For more information about how researchers around the world are working on cardiac simulations, see PIC—Your digital heart: https://www.youtube.com/watch?v=uHdEKZaYP_A
References
[1] ↑ Broadhouse, K. 2019. The physics of MRI and how we use it to reveal the mysteries of the mind. Front. Young Minds. 7:23. doi: 10.3389/frym.2019.00023
[2] ↑ Mac Donald, C., Mukherjee, P., and Yuh, E. 2019. How to see into the brain without surgery? Front. Young Minds. 7:14. doi: 10.3389/frym.2019.00014
[3] ↑ Carter, S., Holder, S., Thijssen, D., and Hopkins, N. 2019. Taking regular breaks from sitting prevents reductions in brain blood flow. Front. Young Minds. 7:77. doi: 10.3389/frym.2019.00077
[4] ↑ Lee, A. W., Crozier, A., Hyde, E. R., Lamata, P., Truong, M., Sohal, M., et al. 2017. Biophysical modeling to determine the optimization of left ventricular pacing site and AV/VV delays in the acute and chronic phase of cardiac resynchronization therapy. J. Cardiovasc. Electrophysiol. 28:208–15. doi: 10.1111/jce.13134
[5] ↑ Rodero, C., Strocchi, M., Marciniak, M., Longobardi, S., Whitaker, J., O’Neill, M. D., et al. 2021. Linking statistical shape models and simulated function in the healthy adult human heart. PLoS Comput. Biol. 17:e1008851. doi: 10.1371/journal.pcbi.1008851