Abstract
Teeth contain a living tissue called dental pulp, enclosed within a hard, outer shell made of enamel and dentin. The dental pulp keeps the teeth alive by providing oxygen, nutrients, and the nerve supply to each tooth. Tooth cavities (also called caries) and injury can destroy the hard shell of the tooth and, when the injury is deep, it can damage the pulp. Infection and inflammation in the pulp can lead to the death of the tooth. With a method called pulp regeneration, scientists aim to bring the life back to a dead tooth. In the near future, it might be possible to regenerate teeth in various shapes and sizes, and even have those new teeth resemble the missing teeth.
What Is a Tooth Made of and What Happens When It Is Damaged?
Imagine a fruit with a hard, outer shell encasing a soft pulp inside. The structure of a tooth is similar, with a hard, outer, white casing made up of substances called enamel and dentin, and a soft inner red pulp (Figure 1). The white part of the tooth, which is visible in the mouth above the gingiva (gums), is called the crown. The part of the tooth that holds it in the bone is called the root. Both the crown and the root have dental pulp in their centers. Dental pulp is rich in blood vessels and nerves, which provide oxygen and nutrients to the tooth, keeping it alive or “vital”. Additionally, our mouths are home to millions of bacteria. Some of these bacteria protect the body, while others eat the sugars present in the mouth and convert it to acid. This acid damages the teeth and causes cavities, which are also called caries. Enamel and dentin are the first barriers against both bacterial infections and other trauma to the teeth, and they protect the dental pulp.

- Figure 1 - A healthy tooth (left) and a tooth damaged by cavities or trauma (right).
- Symptoms of pulpitis, which is inflammation of the tooth pulp, include pain and swelling. This is why regenerative therapies are needed to help patients when a tooth dies. With new, promising, pulp-regenerative approaches, it will be possible to get a new, vital tooth to replace a lost or damaged tooth.
When an injury or infection crosses the initial barrier of dentin and enamel, the pulp activates its repair cells, called stem cells. Stem cells fight infection with the help of immune cells, and they repair the damaged parts of the tooth by regeneration (re-growth) of dentin and bone. During regeneration, the blood vessels in the pulp expand. The pulp starts sending some signals that may be felt as pain or as sensitivity to hot or cold temperatures. Also, the enamel may turn slightly pink. This process of expansion and pain is called inflammation of the pulp, or pulpitis (Figure 1). If the infection/injury is not controlled at this stage, the pulp can expand until it is choked inside the hard, outer case and dies, giving the tooth a grayish-blue color. This is called pulp necrosis. In more severe injuries, the damage and infection may cross the root and spread into the surrounding bone.
The age of a person at the time of a tooth injury is an important factor in deciding the treatment options. In the case of young adults, the careful preservation of healthy or vital pulp is critical for the completion of root formation leading to a healthy tooth. The treatment in this case is called vital pulp therapy, because some vital pulp is left behind. In adults, the root is completely formed, so the infected pulp can be replaced with an appropriate material to block the tooth from further infection and increase its strength. This treatment is called non-vital pulp therapy, because all the pulp is removed.
How Do Dentists Currently Heal and Replace Damaged Teeth?
Over the last decade, rapid progress has been made in the field of pulp therapies to heal injured teeth [1]. As mentioned before, treatment options available to preserve the pulp are called either vital or non-vital pulp therapies. Vital pulp therapy, also called pulp capping, is similar to applying a band-aid with some medicine onto the live pulp. The purpose of vital pulp therapy is to preserve the pulp tissue and keep it healthy, particularly in young adults whose teeth have been partially affected by caries or trauma. Vital pulp therapies are based on the ability of the pulp to repair itself, in the absence of infection [2]. Most commonly, calcium-based medicines are used to treat the pulp in the crown of the tooth and restore its vitality. After healing the pulp, the damaged enamel and dentin are replaced with tooth-colored materials called composites, or silver-containing dark metallic fillings.
Non-vital pulp therapy, also called root canal treatment, refers to the removal and cleaning of the dead, infected pulp from the crown and root of the tooth. In a root canal, the damaged pulp is replaced with a suitable material to provide strength to the tooth. In this treatment, thorough cleaning and disinfection of the root canals is done using various chemicals and cleaning instruments. The clean canal created in the tooth root is then filled with a rubber-like material called gutta-percha, which strengthens the roots when it hardens. Finally, the damaged tooth crown is replaced by an artificial ceramic crown. For infections that have reached the bone, surgeries are carefully performed by drilling a hole in the bone, cutting away the infected part of the root and the surrounding bone, cleaning the area, and covering the damaged area with a calcium-based medicine, for healing. This procedure is called an apicoectomy. The major drawback of non-vital pulp therapies is that, since no vital pulp is left behind, the tooth loses its capacity to repair and regenerate itself. This makes the roots more brittle and prone to fracture, which can cause leakage of the dental chemicals from the root into the bone and can make the tooth prone to greater structural damage [3].
How Is Science Improving the Methods of Healing Damaged Teeth?
In contrast to non-vital pulp therapy, which involves the removal of infected pulp, there are some new experimental therapies that focus on bringing back the lost vital pulp to the tooth, including its blood and nerve supplies. This new approach is called regenerative endodontics, and it consists of 3 basic parts: (1) stem cells to re-grow the missing pulp; (2) a scaffold or matrix to grow the new cells on; and (3) molecules for increasing the growth and formation of the new pulp, called growth and signal factors [4] (Figure 2). By combining these three basic tools, the pulp can be regenerated and the vitality of the tooth can be maintained. Currently, these therapies are performed mostly in laboratories. As scientific advances continue, however, these therapies may be practiced on patients in dental clinics in the future. In laboratories, scientists use various cells from animals and humans to test the new materials and their safety. The findings from these tests are used to develop models that are very similar in function and form to the human tooth and pulp. Such models are called 3D tissue models [5]. The effect of various drugs, dental materials, and treatment procedures can be performed on these models before the new treatments are tested on animals or humans.
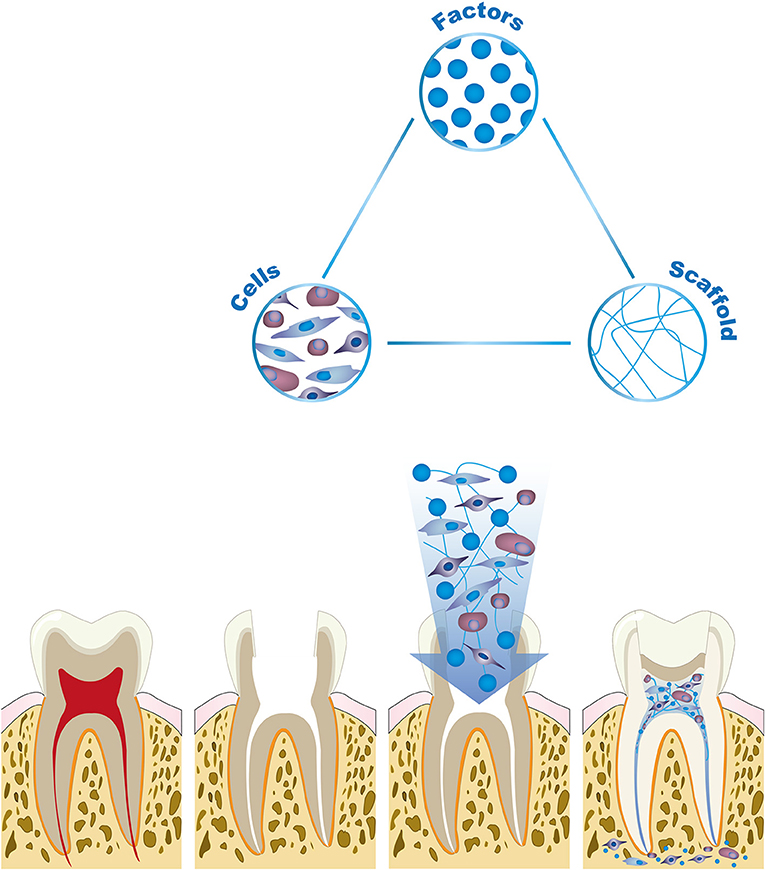
- Figure 2 - Tooth and pulp regeneration is based on tissue engineering research, which aims to rebuild lost body parts and organs.
- The “building blocks” of tooth and pulp regeneration are stem cells, substances (factors) for increasing the growth of the new pulp, and a matrix or scaffold for the cells to grow on. In the future, these strategies will help to generate new pulp for a dead tooth.
Some research is showing that pulp tissue can be regrown even in the absence of a scaffold or matrix [4]. It is also possible that new research will eventually allow the regeneration of not just the pulp, but also the hard, outer shell of the tooth as well! When this approach is ready to be used in patients, it will be a major advancement in the current treatment strategies.
Conclusion: Good News for Damaged Teeth!
With such promising approaches for regenerating tooth pulp, it will be possible give a patient a new, vital tooth to replace a lost or damaged tooth. This new tooth would perform all the functions of a vital tooth. With further advancements in regenerative endodontics and 3D printing, it will be possible to produce teeth in various shapes and forms that will be clones of the missing teeth!
Author Contributions
GO, KJ, and HA were involved in design, literature research, writing, and submission of the manuscript.
Glossary
Regeneration: ↑ The process of total healing after an injury.
Vital Pulp Therapy: ↑ Treatment which aims to preserve and maintain pulp tissue that has been injured but not fully destroyed and bring it back to a live healthy state.
Non-vital Pulp Therapy: ↑ Treatment involving total removal of the pulp and filling of the canal with a suitable material to maintain the tooth in a non-infected state.
Endodontics: ↑ In Greek, Endo means “inside” and Odont means “tooth.” It is the dental specialty concerned with the study and treatment of the dental pulp.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Athanasiadou, E., Paschalidou, M., Theocharidou, A., Kontoudakis, N., Arapostathis, K., and Bakopoulou, A. 2018. Biological interactions of a calcium silicate based cement (Biodentine™) with stem cells from human exfoliated deciduous teeth. Dent. Mater. 34:1797–813. doi: 10.1016/j.dental.2018.09.014
[2] ↑ Dhar, V., Marghalani, A. A., Crystal, Y. O., Kumar, A., Ritwik, P., Tulunoglu, O., et al. 2017. Use of vital pulp therapies in primary teeth with deep caries lesions. Pediatr. Dent. 39:146–59.
[3] ↑ Asgary, S., Fazlyab, M., and Nosrat, A. 2016. Regenerative endodontic treatment versus apical plug in immature teeth: three-year follow-up. J. Clin. Pediatr. Dent. 40:356–60. doi: 10.17796/1053-4628-40.5.356
[4] ↑ Janjić, K., Cvikl, B., Moritz, A., and Agis, H. 2016. Dental pulp regeneration. Int. J. Stomatol. Occl. Med. 8:1–9. doi: 10.1007/s12548-015-0139-1
[5] ↑ Itoh, Y., Sasaki, J. I., Hashimoto, M., Katata, C., Hayashi, M., and Imazato, S. 2018. Pulp regeneration by 3-dimensional dental pulp stem cell constructs. J. Dent. Res. 97:1137–43. doi: 10.1177/0022034518772260